[Gynecological Laparoscopy] 4K laparoscopic salpingo-oophorectomy
Release time: 01 Aug 2023 Author:Shrek
Recently, the non-profit international organization "Ovarian Cancer Research Alliance" launched a "Cancer Prevention Action". One of the contents is to encourage women to preventively remove both fallopian tubes during pelvic surgery. The agency pointed out that 70% of ovarian cancers start in the fallopian tube, and preventive removal of it has been proven to significantly reduce the risk of cancer. Prophylactic removal of fallopian tubes may be a win-win situation. It not only reduces the risk of ovarian cancer, but also preserves the ovary and continues to produce the hormones needed by the body.
How scary is ovarian cancer?
Ovarian cancer is one of the most common malignant tumors in women, and it is also known as the three most common malignant tumors in gynecology together with cervical cancer and endometrial cancer. Epidemiological statistics show that the risk of ovarian cancer in ordinary women is 1 %about. However, its mortality rate ranks first among gynecological malignancies, surpassing the sum of cervical cancer and endometrial cancer, and has become the "silent killer" of women's tumors. Ovarian cancer is difficult to screen for and has a high mortality rate.
Due to the insidious onset, the ovary is located deep in the pelvic cavity, it is difficult to detect the lesion in the early stage and the disease develops rapidly. In addition, there is a lack of effective screening and early diagnosis methods. 70% to 80% of the patients are already advanced ovarian cancer when they see a doctor.
Surgical Indications for Ovarian Cancer
1. Women with a family history of ovarian cancer
2. Middle-aged and elderly women
3. Women with a history of breast, uterine or colorectal cancer
4. Women with BRCA gene mutations (20% of ovarian cancers are caused by gene mutations)
5. Women with endometriosis
6. Women who have difficulty conceiving or have never given birth.
While all surgeries carry some risk, removing the fallopian tubes as part of other gynecological procedures carries few additional risks.
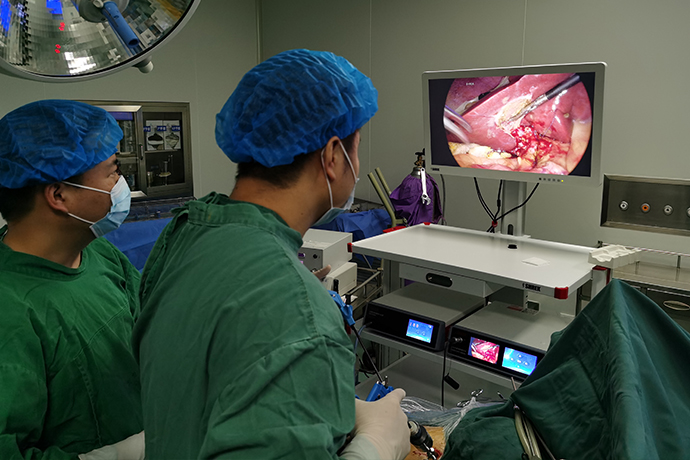
From the actual operation at home and abroad, 4K ultra-high-definition endoscopic minimally invasive surgery will remove the fallopian tube as completely as possible. Generally, it does not increase the risk of infection or bleeding. If the person who simply removed the fallopian tubes wants to have a child again in the future, he can use assisted reproductive technology to fulfill his childbearing desire.
Surgical technical points and precautions
Surgical position: The lithotomy position is generally used. If the uterus has been removed or the uterus is in a suitable position, the supine position can be adopted. Before anesthesia, placing the patient in a proper position and sufficient bedding can protect the patient's joints and limbs.
When the trocar enters the abdomen, the methods can be selected: directly enter the abdomen, enter the abdomen after pneumoperitoneum, and open the abdomen (Hasson type). During surgery, these nerves are damaged in 5 percent of cases).
Although the Hasson maneuver reduces vascular injury, no single modality has been successful in avoiding all possible complications. Under direct vision, insertion of the posterior cannula minimizes damage to the upper abdominal wall vessels.
Note: The line connecting the trocar position should be larger than the contour of the uterus and the position of the adnexal mass, and the specific situation should be analyzed according to the patient's lesion. About 20% to 28% of patients with upper transverse incision of pubic symphysis and more than 40% of patients with lower abdominal median vertical incision have umbilical adhesions. point), or enter the abdomen under the xiphoid process. However, patients with ovarian cysts or masses, suspected severe pelvic infection, and severe endometriosis should avoid entering the abdomen at the upper position for safety reasons.
Anatomical points:
The pelvic cavity has a rich blood supply, and there are left and right common iliac arteries at L3-L5 levels, which are divided into two branches, the internal iliac and the external iliac, at the upper mouth of the pelvis. The internal iliac artery, also known as the "hypogastric artery", is divided into anterior and posterior branches at the distal end, extending to the interior of the pelvic cavity and is responsible for the entire blood supply of the pelvic cavity. The external iliac artery runs along the pelvic wall to the lower part of the groin and becomes the femoral artery. The uterine artery is the anterior trunk branch of the internal iliac artery, which creeps down and anteriorly along the lateral pelvic wall, passes through the base of the broad ligament, and crosses the ureter to the lateral border of the uterus approximately 2 cm lateral to the isthmus.
In general, damage to large blood vessels is rare, with an incidence ranging from 0.01% to 0.64%. The ovarian artery branches from the abdominal aorta, descends to the pelvic cavity along the front of the psoas major muscle, crosses the ureter and the lower part of the common iliac artery, traverses inward with the infundibulum ligament of the pelvis, and enters the ovary through the mesentery of the ovary.
There are several branches in front of the ovarian hilus to supply the fallopian tubes, and their endings are next to the uterine horn, anastomosing with the ascending ovarian branch of the uterine artery. The left and right pelvic structures are different. Due to the existence of the sigmoid colon, the left pelvic infundibulum ligament is relatively difficult to handle. Therefore, in order to fully expose the ligament and uterus on this side, the sigmoid colon often needs to be pushed to the right.
In gynecological surgery, the total injury rate of the urinary tract is about 1% to 2%, and the incidence rate of laparoscopic surgery is higher than that of laparotomy and vaginal hysterectomy. The incidence of ureteral injury alone is 0.05% to 0.5%. Risk factors for genitourinary tract injury include history of pelvic surgery, bleeding, endometriosis, large pelvic mass, and tumor. The most common site of injury to the ureter is near the infundibulum ligament of the pelvis, often when the ligament separates from the pelvic wall. The main measures to prevent injury are clear identification and memory of the surrounding anatomical structures, and sufficient exposure of key parts of the surgical field of view. Preoperative implantation of a ureteral stent can make the ureter easy to identify, but it does not reduce the incidence of ureteral injury during hysterectomy.
In gynecological minimally invasive surgery, the ureter is a retroperitoneal organ, similar in appearance to blood vessels, adjacent to the internal reproductive organs, and divided into the abdominal cavity, pelvic cavity, and bladder wall. The abdominal cavity extends from the renal pelvis to the upper opening of the pelvis. The ovarian artery crosses and descends in the front, and the genital femoral nerve extends to the psoas major in the rear. At the level of the entrance of the pelvis, the right ureter crosses the external iliac artery, and the left and Crossing of the iliac arteries (Luschka's law). The left inferior mesenteric artery runs along the middle of the uterus.
Surgical points:
There are various surgical methods for removing fallopian tubes and ovaries during minimally invasive hysterectomy. The choice of surgical method should be based on the patient's anatomy, pelvic adhesions, and the skill level of the surgeon.
In Baggish & Kerram’s atlas of pelvic anatomy and gynecological surgery, the round ligament is ligated and severed at the beginning of the operation, the Sampson’s artery (an artery composed of branches of the uterine and ovarian arteries, which is parallel to and submerged under the round ligament) is carefully ligated, and the round ligament is carefully separated. Extend the peritoneal incision to the head, incise one side of the broad ligament to expose the ovary and the infundibulum ligament of the pelvis, sufficiently remove the loose connective tissue in the retroperitoneal space to expose the external iliac artery, identify the vascular side and the psoas muscle belly, preferably the iliac Arteries at the bifurcation of the upper mouth of the pelvis.
During minimally invasive surgery, the ureter was identified at the middle lobe of the broad ligament, and it was confirmed that it crossed in front of the bifurcation of the vessels. Lift the ovaries and fallopian tubes with atraumatic forceps, and open a window (cold separation) between the pelvic infundibulum ligament and the uterus with scissors to increase the distance between them. Use bipolar coagulation and ultrasonic scalpel to separate the infundibulum ligament to the uterine horn. , the round ligament can also be used as an indicator of severe pelvic adhesions, and there is no need to separate the round ligament if the uterus is preserved. Careful identification of important anatomical landmarks during surgery can reduce intraoperative complications and unnecessary trauma.
Another approach is to lift the adnexa, carefully dissect the surrounding vessels, pelvic wall, and uterus, perform a peritoneal fenestration to ensure that the pelvic infundibulum has been separated, clamp the pelvic infundibulum under the ovary, and ligate this point at the non-peritoneal fenestration. As shown in Figure 5 and 6. This technique can shorten the operation time, but it also increases the risk of damage to surrounding structures, and it is also prone to ovarian remnant syndrome due to incomplete removal of ovarian tissue. If the pelvic infundibulum ligament cannot be explored due to pelvic adhesions or a large pelvic mass, the uterine-ovarian ligament can be incised appropriately to separate the appendages from the uterus to make room for the removal of the pelvic infundibulum ligament.
When separating the left side, the colon was pushed to the right side with noninvasive forceps, so that the parietal peritoneum had a certain tension, and cold separation was performed along the viscera around the colon. Find the avascular tissue in the retroperitoneum and blunt dissect it as previously described until the psoas muscle is visible. The left pelvic infundibulum ligament should be transected only after the left psoas muscle is seen, and the remaining operations should be performed after the right side has been treated.
If the hysterectomy is not performed during the operation, an endoscopic retrieval bag with a size of 10 mm to 15 mm should be prepared in advance. When the retrieval bag enters the abdominal cavity, a separate opening or an enlarged trocar incision can be used. Removal of the bag from the umbilical cord reduces nerve damage and bleeding. A 15 mm retrieval bag can be attempted without the aid of a cannula to access the abdominal cavity directly through a 10 mm incision, which does not require further enlargement of the incision. If the tumor is cystic, it should be poured into the bag all or part of it at one time. For solid masses, the mouth of the extraction bag should be held at the exit of the abdominal wall with one hand, and the mass should be properly crushed with the other hand to reduce the volume and then removed from the bag. The integrity of the extraction bag should be ensured throughout the process.
In patients with a history of breast cancer or BRCA1/BRCA2 mutations, the ovarian arteries and veins should be carefully ligated 2 cm proximal to the ovary to ensure complete resection of the ovarian tissue. In order to ensure the integrity of the pathology, the ovaries and fallopian tubes should be completely resected and sent for inspection, and a small amount of samples from each ovary should not be sent for inspection.
Care after salpingectomy surgery is as follows:
1. For the care of abdominal wounds, it is recommended to change the dressing frequently to avoid local infection. For laparoscopic surgery, it is recommended that the stitches be removed about 5 days after the operation, and the dressing should not be removed after the stitches are removed, and the dressing should be covered for a few days
2. Dietary care, if the body wants to recover after salpingectomy, it must strengthen nutrition in the diet, and it is also recommended to eat some blood-enriching food, so that the body can recover as soon as possible
3. After salpingectomy, local care of the vulva should be done, especially during the catheterization period, it is recommended to strengthen care to avoid urinary tract infection
4. If there may be a small amount of bleeding or no bleeding in the vulva, wipe the vulva 1-2 times a day to reduce the possibility of infection.

- Recommended news
- 【General Surgery Laparoscopy】Cholecystectomy
- Surgery Steps of Hysteroscopy for Intrauterine Adhesion
- [ENT Surgery: Nasal Endoscopy] Endoscopic Treatment of Nasal Polyps
- [Otolaryngology Nasal Endoscopy] Methods and Precautions for Nasal Bleeding Control under Nasal Endoscopy
- [Orthopedic UBE Section] Four Years of Evolution of UBE Technology: From Lumbar Fusion to the "Forbidden Zone" of Thoracic and Cervical Spine, and the Unignorable "Hydraulic Pressure Crisis"