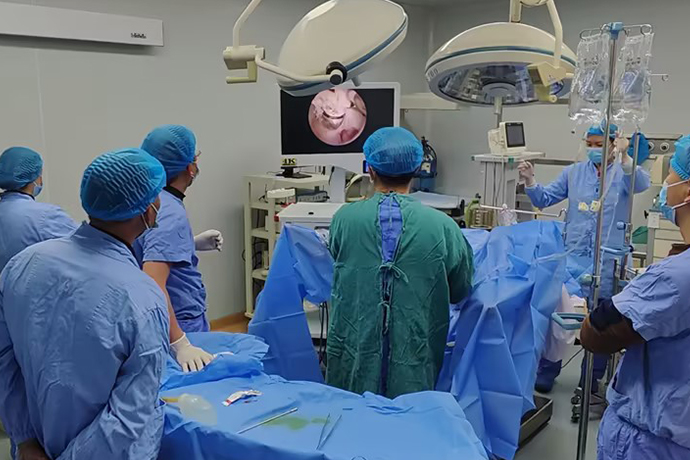
[Gynecological Hysteroscopy] Techniques for Preventing and Treating Complications of Hysteroscopic Surgery
Release time: 02 Dec 2025 Author:Shrek
Hysteroscopic diagnosis and treatment of intrauterine lesions is minimally invasive and effective. However, due to the need for energy equipment, distension media, intrauterine pressure, and the limited surgical space and inability to suture, hysteroscopic surgery presents different complications compared to traditional surgery, even posing a risk of death. Common complications include uterine perforation, bleeding, fluid overload, hyponatremia, air embolism, and postoperative uterine rupture. This article will discuss the causes and prevention methods of hysteroscopic surgical complications to improve the safety of hysteroscopic surgery.
I. Bleeding
The endometrium has a rich blood supply. During endometrial resection, to avoid bleeding, the cutting depth must be ensured to be 2-3 mm below the endometrium. The main cause of intraoperative bleeding during hysteroscopic surgery is the deep destruction of the myometrial tissue beneath the endometrium.
High-risk factors: Uterine perforation, arteriovenous fistula, placenta accreta, cervical pregnancy, cesarean scar pregnancy, and coagulation disorders, etc.
Countermeasures: Preoperative drug pretreatment (administration of oxytocin and hemostatic agents), intrauterine balloon compression, combined laparoscopic monitoring, and prophylactic uterine artery occlusion, etc.
The treatment plan is determined based on the amount, location, extent of bleeding, and type of surgery.
II. Uterine Perforation
High-risk factors: Cervical stenosis, history of cervical surgery, excessive uterine flexion, small uterine cavity, and inexperienced surgeon, etc.
Clinical manifestations: ① Uterine cavity collapse, obscured vision;
② B-ultrasound images show free fluid around the uterus, or a large amount of irrigation fluid entering the abdominal cavity;
③ Hysteroscopy reveals the peritoneum, intestines, or greater omentum;
④ If laparoscopic monitoring is used, a clear uterine serosal surface, blistering, bleeding, hematoma, or perforation may be visible;
⑤ The electrode may enter and damage pelvic and abdominal organs, causing corresponding complications and symptoms, etc.
Countermeasures: Carefully locate the perforation site and determine the treatment plan.
① Fundus perforation: The uterine fundus muscles are thickened with relatively few blood vessels, resulting in minimal bleeding. Oxytocin and antibiotics can be used for observation.
② Lateral wall and isthmus perforation: This may damage uterine blood vessels, requiring immediate exploratory laparotomy. Bleeding at the perforation site can be controlled laparoscopically with bipolar electrocoagulation. Larger perforations require suturing.
③ Unclear situation: Laparoscopy should be performed even if the patient's overall condition is normal to observe for bleeding and its source.
④ Postoperative pain management: Pain management within 24 hours post-surgery requires comprehensive examination. If uterine perforation is suspected, laparoscopy should be performed promptly.
Prevention: ① Strengthen cervical pretreatment and avoid forceful cervical dilation. If the patient is postmenopausal, cervical softening medication such as misoprostol should be administered preoperatively. If the patient has cervical stenosis, cervical dilation medications should be used to ensure successful hysteroscopy insertion.
② Ultrasound or laparoscopy may be used as appropriate to clarify the lesion location and obtain a clear surgical field.
③ Surgical skills should be trained and improved.
④ GnRH-α drugs may be used as appropriate to shrink fibroids or uterine volume and thin the endometrium.
III. Excessive Irrigation Fluid Absorption Syndrome
During hysteroscopic surgery, the distension pressure and use of non-electrolyte irrigation media can cause fluid to enter the patient's body. When this exceeds the body's absorption threshold, a series of symptoms and signs may occur.
Clinical manifestations include bradycardia, elevated or decreased blood pressure, nausea, vomiting, headache, blurred vision, restlessness, mental confusion, and drowsiness. If not treated promptly, convulsions, cardiopulmonary failure, and even death may occur.
Triggering factors: Intrauterine hypertension, excessive absorption of perfusion media, prolonged surgical time, etc.
Countermeasures: Oxygen therapy, diuresis, treatment of hyponatremia, correction of electrolyte imbalance and water intoxication, management of acute left ventricular failure, prevention and treatment of pulmonary edema and cerebral edema.
Special attention should be paid to correcting dilutional hyponatremia. Sodium supplementation should be calculated and administered according to the following formula: Required sodium supplementation = (Normal serum sodium value - Measured serum sodium value) 52% × Body weight (kg). The initial supplementation dose should be 1/3 or 1/2 of the calculated total. Subsequent supplementation doses should be determined based on changes in the patient's level of consciousness, blood pressure, heart rate, pulmonary signs, and serum Na+, K+, and Cl- levels. Rapid, high-concentration intravenous sodium supplementation should be avoided to prevent a temporary state of low osmotic pressure in the brain, causing fluid to shift from the interstitial spaces of brain tissue into the blood vessels, leading to brain dehydration and brain damage.
Hysteroscopic bipolar systems use physiological saline as the intrauterine irrigation medium, reducing the risk of hyponatremia, but the risk of fluid overload remains.
Prevention: ① Cervical and endometrial pretreatment helps reduce irrigation fluid absorption;
② Maintain intrauterine pressure ≤ 100 mmHg or < mean arterial pressure;
③ Control the irrigation fluid difference between 1000 and 2000 ml;
④ Avoid excessive damage to the uterine wall.
IV. Gas Embolism
Gas embolism is a very rare but fatal complication of hysteroscopic surgery. During hysteroscopic surgery, air can enter the uterine cavity through the irrigation system's inlet tube, cervix, repeatedly inserted dilators, and hysteroscopic instruments, and enter the venous system through intraoperatively opened sinuses. Gas can enter the inferior vena cava, then the right heart, pulmonary artery, and ultimately the lungs, causing pulmonary hypertension, hypoxemia, circulatory failure, and cardiac arrest.
During surgical procedures, tissue vaporization and room air may enter the venous circulation through open blood vessels in the uterine cavity, leading to gas embolism. Gas embolism has a sudden onset and rapid progression. Early symptoms include decreased end-tidal PCO2, bradycardia, decreased PO2, and a loud water murmur heard in the precordial area. This is followed by increased blood flow resistance, decreased cardiac output, cyanosis, hypotension, tachypnea, and cardiopulmonary failure, ultimately resulting in death.
Countermeasures: Immediately stop the procedure, administer positive pressure oxygen, and correct cardiopulmonary failure. Simultaneously, administer normal saline to promote blood circulation, place a central venous catheter, and monitor cardiopulmonary artery pressure.
Specific measures: ① The mechanical pump used for intraoperative distending fluid injection should be equipped with a Y-connector to prevent air from entering the infusion tubing. ② Set a reasonable distending fluid pressure; as mentioned earlier, the distending fluid pressure should generally not exceed 100 mmHg, while controlling the volume of distending fluid used. ③ During electrocautery, tissue vaporization can generate a significant amount of gas; using cold-blade instruments or minimizing surgical time can reduce gas production. ④ After cervical dilation, the surgeon must maintain a closed cervix during the procedure to avoid repeated insertion and removal of instruments from the uterine cavity. ⑤ Rapid intraoperative identification: Anesthesiologists should pay close attention to monitoring end-tidal carbon dioxide partial pressure during hysteroscopy, as a decrease in end-tidal carbon dioxide partial pressure is a sensitive early indicator of gas embolism. ⑥ Once gas embolism is detected, the surgery should be stopped immediately, the uterine fluid emptied, and a moist gauze placed in the vagina to prevent gas from entering. Immediately position the patient head-up, elevating the heart to reduce gas entry.
Prevention:
① Avoid head-down, hip-up position;
② Empty the air from the infusion tubing before surgery;
③ Perform cervical pretreatment to avoid rough dilation that could cause cervical laceration;
④ Strengthen intraoperative monitoring and emergency treatment.
V. Prevention of Intrauterine Adhesions
① Using a needle electrode to incise the mucosa and capsule of the protruding fibroid within the uterine cavity, and then using a ring electrode to cut the fibroid, minimizing damage to the surrounding normal endometrium is key to preventing secondary intrauterine adhesions after surgery. ② If there is a large exposed wound in the uterus or if preoperative GnRH-a treatment has resulted in low estrogen levels, appropriate postoperative estrogen can stimulate endometrial growth, accelerate epithelialization, and prevent intrauterine adhesions.
③ An IUD can also be placed at the end of the procedure. If there is significant bleeding during the procedure, it can be placed after menstruation resumes postoperatively. The physical support provided by the IUD helps prevent intrauterine adhesions.
VI. Infection
Causes: ① The doctor did not strictly follow aseptic procedures during the surgery;
② No rigorous examination of pelvic and vaginal secretions was performed preoperatively.
Prevention: ① Strictly adhere to surgical indications;
② Surgery is contraindicated during the acute phase of reproductive tract infections;
③ Postoperative antibiotics should be used as appropriate to prevent infection.
VII. Treatment Failure and Recurrence
Treatment failure or symptom recurrence can be considered for subsequent treatments, including a second hysteroscopic surgery, medication, or hysterectomy. It is particularly emphasized that hysteroscopic surgery is a conservative procedure for treating uterine diseases. Informed consent must be fully obtained before the procedure, and surgery must never be performed against the patient's will.
Two common misconceptions: Have you fallen for any of them?
Misconception 1: Is electrocautery more likely to damage the endometrium?
Regardless of the instrument used, linear incision and local removal of lesions are preferred, resulting in minimal damage to the endometrium and no large-scale loss of endometrial tissue. Therefore, there is no difference in the impact of electrocautery and cold knife surgery on the endometrium, and the postoperative success rate or natural pregnancy rate is the same. Therefore, there is no need to worry about electrocautery.
Misconception 2: Will scraping the endometrium during hysteroscopy thin the endometrium?
The answer is no.
The purpose of hysteroscopy, in addition to visually examining the morphology of the uterine cavity and checking for lesions, is to evaluate the endometrium. Endometrial evaluation includes visual examination of endometrial thickness, color, and glandular openings, as well as taking endometrial tissue for microscopic examination to check for pathological changes and rule out cancerous changes. This examination is essential.
One point needs clarification: what we call "hysteroscopic curettage" should actually be called "endometrial preparation" or "endometrial sampling." The purpose is to scrape a small amount of endometrial tissue for pathological examination and to stimulate the release of cytokines that promote embryo implantation. It is not a traditional "curettage procedure," so it does not thin the endometrium!

- Recommended news
- 【General Surgery Laparoscopy】Cholecystectomy
- Surgery Steps of Hysteroscopy for Intrauterine Adhesion
- [ENT Surgery: Nasal Endoscopy] Endoscopic Treatment of Nasal Polyps
- [Otolaryngology Nasal Endoscopy] Methods and Precautions for Nasal Bleeding Control under Nasal Endoscopy
- [Orthopedic UBE Section] Four Years of Evolution of UBE Technology: From Lumbar Fusion to the "Forbidden Zone" of Thoracic and Cervical Spine, and the Unignorable "Hydraulic Pressure Crisis"