[Gynecological Hysteroscopy] Hysteroscopic Adhesiolysis
Release time: 25 Nov 2025 Author:Shrek
In the treatment of infertility, some patients are often required to undergo hysteroscopy and treatment for various reasons.
While hysteroscopy is a minor procedure, many patients often feel anxious about it. The most common questions include: "Doctor, why do I need this? Is it painful? Can I skip it? Is conservative treatment sufficient?" Some compare the mother's uterus to a cradle for the baby's peaceful sleep, while others liken the endometrium to soil nurturing seed germination. Before placing the baby in the cradle, we typically lay a blanket to ensure it's thick enough and check for any unwanted objects.

Just as we prepare soil by weeding, tilling, watering, and fertilizing before planting seeds, the same preparation applies to preparing the uterus for transplantation. Beyond fertilization and irrigation, other tasks like examining the uterine lining and removing weeds require specialized techniques—hysteroscopy.
01
What is a hysteroscope?
Hysteroscopy is a light-based endoscopic procedure used to diagnose infertility causes, identify uterine cavity lesions, and perform treatments with follow-up. It not only determines the location, size, appearance, and extent of lesions but also enables detailed observation of surface tissue structures. Under direct visualization, it allows for tissue sampling or targeted curettage to remove lesions, significantly improving diagnostic accuracy for intrauterine diseases. This method has evolved to address the limitations of traditional diagnostic and therapeutic approaches.
As a minimally invasive procedure, hysteroscopy can generally be performed in outpatient settings. The entire process involves intravenous anesthesia, leaving the patient unconscious for approximately 10-30 minutes. The complexity and duration of the procedure vary significantly. Hysteroscopy is indicated for any suspected intrauterine lesions requiring diagnosis and treatment.
02
When is hysteroscopy needed
01
abnormality of uterine cavity
This is a common gynecological condition. Polyps, caused by localized excessive endometrial growth, appear as single or multiple smooth masses protruding into the uterine cavity. They may lead to irregular vaginal bleeding and infertility. Ultrasound examinations may reveal endometrial polyps, uneven endometrial echoes, or endometrial thickening. Before undergoing in vitro fertilization (IVF), if endometrial hyperplasia or polyps are detected, a hysteroscopy should be performed first to prevent potential issues with embryo implantation.
Endometrial polyps under hysteroscopy
The incidence of endometrial polyps in infertile patients ranges from 14.9% to 26.5%. Traditional ultrasound examinations may miss small endometrial polyps, whereas hysteroscopy allows direct visualization for diagnosis, evaluation, treatment, and biopsy.
02
intrauterine adhesious :
Uterine adhesions can significantly reduce embryo implantation rates, particularly in severe cases. Therefore, hysteroscopic adhesion lysis is required before embryo transfer to separate the adhesions. For mild adhesions, a replacement cycle of 1-3 months is recommended post-surgery. In cases of moderate to severe adhesions, a contraceptive ring may be placed to prevent re-adhesion, followed by hysteroscopic removal of the ring or placement of a balloon in the uterine cavity, which is typically removed one week after the procedure. Notably, severe adhesions may require multiple surgical interventions.
For some patients with infertility, hysteroscopy can also be used to observe the anatomical morphology of the fallopian tube opening and to determine the patency of the fallopian tube by inserting a tube and flushing it.
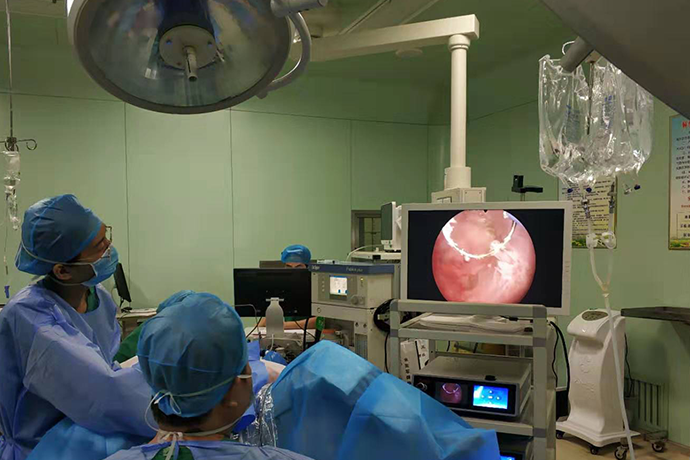
The steps of hysteroscopic adhesiolysis
(1) After bladder distension, carefully position the probe under B-mode ultrasound guidance and dilate the cervix and uterine cavity sequentially using a dilator. If the probe cannot reach the uterine fundus or only penetrates the cervical canal in cases of uterine atresia, the procedure may be deferred for hysteroscopic intervention. Alternatively, under B-mode ultrasound guidance, the probe can be advanced forcefully along the cervical and uterine midline toward the fundus.
2) Under B-mode ultrasound guidance, the hysteroscope was inserted into the uterine cavity through the external cervical os and cervical canal. The morphology of the cervical canal and uterine cavity was examined, bilateral uterine horns and fallopian tube openings were observed, and adhesion tissues were exposed to determine the location and severity of adhesions.
2) Under B-ultrasound guidance, the hysteroscope was inserted into the uterine cavity along the external cervical os and cervical canal. The morphology of the cervical canal and uterine cavity was examined, bilateral uterine horns and fallopian tube openings were observed, and adhesion tissues were exposed to determine the location and severity of adhesions.
3) The dense adherent scar tissue in the cervical canal can be incised with the needle electrode or excised with the loop electrode of the hysteroscopic resection instrument
4) Central membranous or fibrous adhesions in the uterine cavity may be excised using a hysteroscopic needle electrode or a loop electrosurgical unit (ESU) . During the procedure, care must be taken to preserve the normal endometrial tissue.
5) For adhesion scar tissue on the anterior, posterior, and lateral walls of the uterine cavity, a needle electrode can be used to incise along the uterine long axis, and a loop electrode may be employed for excision when necessary.
6) Adhesions in the fundus and cornua of the uterus require transverse incision using a needle electrode or circumferential cutting with a loop electrode to fully open the uterine fundus (Fig. 7-7A, B). Simultaneously, the incision should extend toward the cornua, aiming to expose the fallopian tube openings by maximizing bilateral cornual exposure. Under B-mode ultrasound guidance, the adhesion band at the cornual angle is typically separated with a needle electrode, supplemented by loop electrode cutting when necessary. This step-by-step approach restores the normal morphology of both cornua and fallopian tube openings (Fig. 7-8A-F), with particular care to preserve the normal endometrial tissue at the cornual are
7) For patients with uterine wall scar spasm causing uterine cavity narrowing, needle electrodes can be used to make 4-5 longitudinal radial incisions along the uterine long axis to expand the uterine cavity volume (Figure 7-9).
8) For cases with a closed uterine cavity where the endoscope's front end is blind, under B-mode ultrasound guidance, a needle electrode or loop electrode can be gently advanced along the cervical and uterine midline to attempt to separate adhesions, creating a passage to expose the uterine cavity (Fig. 7-10A~C). Subsequently, follow the aforementioned steps to excise the intrauterine adhesions and restore the normal uterine cavity morphology (Fig. 7-10D).
9) After the procedure, the objective lens was retracted to the internal os of the cervix to observe the morphology and symmetry of the uterine cavity.
(10) For laparoscopic supervision, methylene blue solution can be injected into the uterine cavity to perform a fallopian tube patency test, with the patency of the fallopian tubes observed under laparoscopy (Figure 7-12).
(2) Hysteroscopic scissors separation of intrauterine adhesions (1) First, perform hysteroscopy. Insert a hysteroscopic treatment scope to visually examine the uterine cavity morphology and adhesion status. (2) Deliver a flexible semi-rigid or rigid scissors along the operational channel of the hysteroscopic treatment scope into the uterine cavity.
(3) Using hysteroscopic scissors, gradually separate the adhesions from the center of the uterine cavity outward to expand the uterine cavity (Figure 7-13). For extensive adhesions, pay attention to the depth of adhesion separation and be vigilant for potential uterine perforation. When reaching the pubic symphysis, under B-mode ultrasound guidance, try to mobilize the uterine angle to expose the fallopian tube openings.
4) When the uterine cavity or cervical canal is completely closed, the separation should be started from the adhesion below and gradually along the midline of the uterus under the guidance of B-mode ultrasound until a new uterine cavity is opened.
Hysteroscopic cannulation of the fallopian tube opening
03
abnormal cervix
1. Cervical polyps: If detected before IVF, hysteroscopic removal is recommended as these polyps may obstruct the cervix, causing difficulties in embryo transfer or bleeding. Moreover, post-pregnancy bleeding from polyps can be difficult to distinguish from intrauterine bleeding.
2. Cervical adhesions: Intrauterine procedures may cause cervical trauma, leading to adhesions that can complicate embryo transfer. In such cases, hysteroscopy is required to separate the adhesions.
03
Gynecological-related diseases
Some diseases related to gynecology need to be examined through hysteroscopy, such as
1. Abnormal uterine bleeding: such as excessive menstruation, frequent menstruation, prolonged menstruation, irregular vaginal bleeding, should be performed hysteroscopy after excluding pregnancy.
2. Patients receiving hormone replacement therapy or with oligomenorrhea: Prolonged hormone therapy or infrequent menstruation (e.g., in polycystic ovary syndrome) may cause endometrial hyperplasia and polyp formation, which in severe cases could lead to endometrial cancer. Therefore, hysteroscopy is required for evaluation.
04
unexplained infertility, recurrent miscarriage
It is recommended to perform hysteroscopy to exclude abnormalities that cannot be detected by imaging examinations.
05
hydrops tubae
Hydrosalpinx is a key factor affecting embryo implantation. The conventional surgical approach involves laparoscopic salpingectomy or ligation, which requires hospitalization and general anesthesia. Hysteroscopic salpingocystectomy, however, is performed under direct visualization using a micro-coil placed in the interstitial part of the fallopian tube to prevent fluid reflux into the uterine cavity.
The procedure is short (about 10-20 minutes), simple to perform, and less expensive than laparoscopy, but IVF treatment can only be performed 2-3 months after the surgery.
06
Other rare cases
If the location of the cleft is difficult to transplant, the location and depth of the diverticulum should be determined by hysteroscopy to guide the next embryo transfer.
07
embryonic repeated implantation failure
Repeated implantation failure refers to cases where ≥3 high-quality embryo transfers fail or a cumulative total of ≥10 embryo transfers fail. Although ultrasound may indicate no significant endometrial abnormalities, hysteroscopy is recommended to rule out endometrial issues that ultrasound may not detect, such as mild intrauterine adhesions.
Even if no abnormalities are found by hysteroscopy, mild scraping can stimulate the endometrium and improve the endometrial environment, which may make the next embryo transfer more likely to implant.
Hysteroscopy operation time and precautions
·
Hysteroscopic surgery can be performed after menstrual bleeding has completely stopped. If tubal flushing is performed, it should be done no later than 5 days after menstruation ends, otherwise the endometrium may become too thick, and edema may occur after uterine dilation, which could impair the surgical view.
·
·
Depending on the endometrial condition of the patient, the attending physician decides when to perform the procedure during the menstrual cycle.
·
·
Sexual intercourse was prohibited for 3 days before the operation.
·
·
Avoid greasy food and overeating before surgery, and drink less water.
·
·
The operation lasted from 10 minutes to half an hour.
·
·
If you need anesthesia, ask for a family member to accompany you.
·
·
No bed rest was required after operation, but no overwork was allowed.
·
·
Eat a normal diet and avoid spicy and blood-activating foods.
·
·
If you have an intrauterine device (IUD) and experience symptoms like lower back pain, a sensation of heaviness, or light spotting, these are normal and do not require medical attention. However, if you experience severe abdominal pain or heavy, continuous bleeding, you should seek medical examination. If no discomfort is present, you can resume your usual fitness activities.
·
·
Patients who have undergone intrauterine device (IUD) insertion should return to the center for IUD removal after their second menstrual period ends. If the bleeding is not completely stopped and only brown discharge is present without fresh blood, the procedure can proceed.
·
Video of hysteroscopy technique abroad
Prevention and treatment of complications in hysteroscopic surgery
NO1. Uterine perforation
(1) Causes: The high risk factors for uterine perforation include cervical stenosis, history of cervical surgery, excessive uterine flexion, small uterine cavity, and lack of experience in surgical procedures.
(2) Clinical manifestations: ① Uterine cavity collapse with blurred visual field. ② Ultrasound reveals free fluid around the uterus or significant peritoneal effusion. ③ Hysteroscopy demonstrates peritoneal, intestinal, or omental structures. ④ With laparoscopic monitoring, the serosal surface may appear translucent, blistered, hemorrhagic, hematoma-affected, or perforated. ⑤ The application of electrodes may damage pelvic and abdominal organs, causing corresponding complications.
(3) Management: ① First, locate the perforation site and assess adjacent organ damage to determine the treatment strategy. ② If there is no active bleeding or organ damage, administer oxytocin and antibiotics with observation. ③ For extensive perforations involving vascular injury or organ damage, immediate laparoscopic or open exploration should be performed with appropriate intervention.
(4)Prevention:①Enhance cervical preparation and avoid violent dilation. ②Combine with ultrasound or laparoscopic surgery when appropriate. ③Improve the surgeon's skills. ④Use GnRH-a drugs to reduce the size of fibroids or uterus and thin the endometrium when necessary.
NO2. Bleeding
(1) Main reason: the submucosal muscle tissue was destroyed too deeply.
(2) The high risk factors of hemorrhage included: uterine perforation, arteriovenous fistula, placenta implantation, cervical pregnancy, cesarean scar pregnancy and coagulation disorders.
(3) Management: ① For persistent cervical bleeding due to poor uterine contraction, apply gauze soaked in posterior pituitary vasopressin dilution solution (30ml saline + 20U vasopressin) to induce uterine contractions. Remove the tamponade 8-12 hours post-procedure. ② When deep uterine blood vessels are incised and electrocoagulation fails, place a Foley catheter with balloon retention. Normal uterine cavity capacity is 5-10ml; for severe hemorrhage in larger uteruses, 15-30ml may be injected. Patients with uterine fibroids require 30-60ml. The balloon's expansion ensures uniform pressure on the uterine wall, achieving effective hemostasis. Typically, 12-24 hours of balloon retention suffices. Concurrent antibiotic prophylaxis is advised to prevent infection.
(4) Prevention: ① Minimize endometrial thickness to facilitate resection, such as through preoperative medication or performing a curettage before endometrial resection. ② Ensure adequate perfusion flow rate to maintain clear surgical visualization. ③ Endometrial resection should be performed 2-3mm below the endometrium. Since the vascular layer of the uterine muscle wall is located 5-6mm beneath the endometrium, excessive resection may damage blood vessels, causing uncontrollable hemorrhage. ④ Create smooth surgical surfaces to clearly identify bleeding vessels. For poorly visible hemorrhagic points hidden within tissues, blind electrocoagulation often proves ineffective. Instead, excise elevated tissues to expose bleeding sites before hemostasis. ⑤ Follow sequential resection: complete hemostasis at each site before proceeding to the next. Avoid excessive wound size and blood loss. Multiple bleeding points may blur the surgical field and hinder procedures.
NO3. Gas embolism
(1) Reason: The tissue vaporization and the air in the operating room may enter the venous circulation through the open blood vessels in the uterine cavity, leading to gas embolism.
(2) Clinical manifestations: Gas embolism has sudden onset and rapid progression. Early symptoms include decreased end-tidal PCO2, bradycardia, decreased PO2, and audible large waterwheel murmur in the precordial area. Subsequently, increased blood flow resistance and reduced cardiac output lead to cyanosis, hypotension, tachypnea, and ultimately death due to cardiopulmonary failure.
(3) Treatment: Immediately stop the operation, administer positive pressure oxygen, and correct cardiopulmonary failure. Simultaneously, administer normal saline to promote blood circulation, place a central venous catheter, and monitor cardiopulmonary artery pressure.
(4)Prevention:①Avoid the position of head lower than the buttocks. ②Drain the gas in the water pipe before the operation. ③Pre-treatment of the cervix to avoid the injury of the cervix caused by the rough dilatation. ④Strengthen the inoperative monitoring and emergency treatment.
NO4. Overabsorption syndrome of irrigation fluid
(1) Reason: In hysteroscopy, the pressure of the balloon and the use of non-electrolyte perfusion medium can make the liquid medium enter the patient's body. When it exceeds the threshold of human absorption, it can cause fluid overload and dilutional hyponatremia, and cause corresponding changes in the heart, brain, lung and other important organs, and a series of clinical symptoms.
(2) Clinical manifestations: including hypertension or hypotension, slow heart rate, nausea, vomiting, headache, blurred vision, restlessness, mental confusion and drowsiness, etc. If not treated in time, convulsions, cardiopulmonary failure and even death will occur.
(3) Inducing factors: high intrauterine pressure, large amount of perfusion medium absorption, etc.
(4) Management: ① Administer oxygen therapy, diuretics, treat hyponatremia, and correct electrolyte imbalances and water intoxication. ② Manage acute left heart failure and prevent pulmonary and cerebral edema. ③ Special attention should be given to correcting dilutional hyponatremia, calculated using the sodium supplementation formula: Required sodium supplementation = (Normal blood sodium level-Measured blood sodium level) × 52% × Body weight (kg). ④ The hysteroscopic bipolar electric system uses normal saline as the intrauterine perfusion medium, reducing the risk of hyponatremia but still posing the risk of fluid overload.
(5)Prevention: ①Pre-treatment of cervix and endometrium can reduce the absorption of perfusion fluid. ②Maintain uterine cavity pressure ≤100mmHg or <mean arterial pressure. ③Control the difference of perfusion fluid at 1000-2000ml. ④Avoid excessive damage to uterine muscle wall.
NO5. Preventive measures for intrauterine adhesions:
①Using a needle electrode to incise the mucosa and capsule of the protruding uterine fibroid, followed by a loop electrode to excise the tumor, while minimizing damage to the surrounding healthy endometrium, is crucial for preventing postoperative secondary intrauterine adhesions. ②For larger exposed lesions or patients with preoperative GnRH-a-induced low estrogen levels, postoperative estrogen supplementation can stimulate endometrial growth, accelerate epithelialization, and prevent adhesions. ③An intrauterine device (IUD) may also be placed during surgery. If significant intraoperative bleeding occurs, the IUD can be retained after the postoperative menstrual cycle to provide physical support and prevent adhesions.
NO6. Infection
Strictly control the indications of operation, the operation is contraindicated in the acute phase of reproductive tract infection, and antibiotics should be used after operation to prevent infection.
- Recommended news
- 【General Surgery Laparoscopy】Cholecystectomy
- Surgery Steps of Hysteroscopy for Intrauterine Adhesion
- [ENT Surgery: Nasal Endoscopy] Endoscopic Treatment of Nasal Polyps
- [Otolaryngology Nasal Endoscopy] Methods and Precautions for Nasal Bleeding Control under Nasal Endoscopy
- [Orthopedic UBE Section] Four Years of Evolution of UBE Technology: From Lumbar Fusion to the "Forbidden Zone" of Thoracic and Cervical Spine, and the Unignorable "Hydraulic Pressure Crisis"