[Gynecological Hysteroscopy] IUD Removal under Hysteroscopy
Release time: 20 Nov 2025 Author:Shrek
The term "IUD" is familiar to everyone; medically, it's called an "intrauterine device."

In the 1970s and 80s, family planning was a fundamental national policy. Many women opted for IUDs for contraception, as it didn't affect future pregnancies and provided easy contraception. Statistics show that from 1980 to 2009, Chinese women used IUDs 286 million times. Three or four decades later, those women who had IUDs inserted are now entering menopause. Due to neglect and a lack of knowledge about IUDs, many women still don't realize that IUDs are not a "one-and-done" solution and require regular checkups to check for displacement or expulsion. Otherwise, it can seriously harm their health.
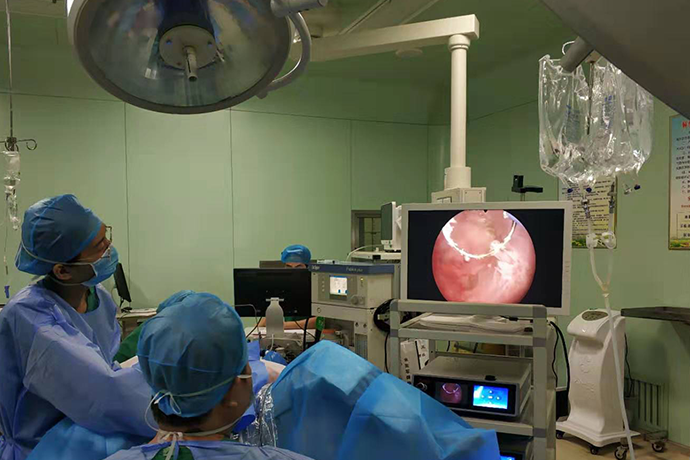
A hysteroscopy is an endoscope using a fiber optic light source. Hysteroscopy involves using a distending medium to dilate the uterine cavity and inserting a fiber optic speculum through the vagina to directly visualize the physiological and pathological changes of the cervical canal, internal cervical os, uterine cavity, and fallopian tube openings. This allows for direct and accurate sampling of lesion tissue for pathological examination. Hysteroscopic surgery can also be performed directly under hysteroscopic guidance. It offers advantages such as clear visualization, high lesion identification, minimal trauma, rapid postoperative recovery, and the ability to be performed as a day surgery, making it widely used in hospitals at all levels. Hysteroscopy and related surgeries have become an almost unavoidable hurdle for female patients.
Hysteroscopy is used to remove difficult-to-remove intrauterine devices (IUDs). This is often due to excessive menstrual bleeding or two or more failed attempts at IUD removal during family planning. Hysteroscopy reveals that the IUD is twisted, deformed, or broken; some are only remnants, some are implanted in the myometrium, and some have migrated outside the uterine cavity. Hysteroscopy allows direct observation of the IUD's morphology and location within the uterine cavity, determining whether it is implanted in the uterine wall, thus deciding the route and method of IUD removal.
Common side effects or complications after IUD insertion include:
1. Abnormal uterine bleeding and pain;
2. IUD embedding or displacement;
3. Perforation;
4. Pregnancy with an IUD in place (meaning pregnancy and IUD coexisting).
Situations where intrauterine device (IUD) insertion is not recommended:
1. Acute pelvic inflammatory disease; acute vaginitis;
2. Severe cervical erosion, menorrhagia or irregular bleeding, uterine fibroids, or a narrow cervix;
3. Women with serious systemic diseases should also avoid IUD insertion, as it may worsen inflammation or increase menstrual flow.
When should an IUD be removed?
1. Those who have had an IUD for 5-10 years and wish to replace it with a new one.
2. Those experiencing irregular vaginal bleeding or other symptoms that are unresponsive to treatment. Heavy vaginal bleeding or bleeding accompanied by infection requires immediate removal.
3. Those who wish to have more children.
4. Those who have undergone sterilization for one year. Removal is recommended for those who have been menopausal for more than six months.
5. Those experiencing severe side effects and wishing to change contraceptive methods.
6. Those who become pregnant while using an IUD; it can be removed during an abortion.
Intrauterine device (IUD) displacement refers to:
the IUD leaving its normal position within the uterine cavity and becoming partially or completely embedded in the myometrium, or displaced into the abdominal cavity, broad ligament, bladder, rectum, or other locations. When an IUD becomes displaced, it not only loses its contraceptive function but also causes problems for the user.
Symptoms of intrauterine device displacement:
1. Abdominal pain;
2. Pregnancy with the IUD in place;
3. Prolonged menstrual bleeding.
Causes of IUD displacement:
1. Increased risk of displacement during breastfeeding;
2. IUD is too large or improperly placed;
3. IUD shape is not compatible with the uterine cavity.
Based on the degree of ectopic placement, IUDs can be classified into three categories:
(1) Partial embedding: The IUD is partially embedded in the endometrium and myometrium.
(2) Complete embedding: The IUD is completely embedded in the myometrium or mostly embedded in the myometrium with some exposed serosal layer.
(3) Extrauterine IUD placement: The IUD is located outside the pelvic cavity, abdominal cavity, bladder, intestines, broad ligament, or peritoneum.
Case Study: Ms. Chen used an intrauterine device (IUD) for contraception after giving birth to her second child six years ago. Recently, she experienced frequent lower abdominal pain and occasional light vaginal bleeding over the past two months. Ms. Chen went to the hospital for an ultrasound examination, which revealed that the IUD was embedded in the uterine muscle layer. In other words, the IUD was not functioning properly and had become embedded in the uterine muscle, requiring surgical removal.
Sensing the seriousness of the situation, the doctor quickly arranged a hysteroscopy. Under the endoscope, it was clear that the IUD, shaped like a "V," was deeply embedded in the uterine horn muscle layer. Performing a conventional IUD removal procedure in this condition would be very dangerous; blind removal could lead to failure, increasing patient suffering, and uterine perforation could have extremely serious consequences.
Therefore, a hysteroscopic IUD removal was performed. With direct visualization of the uterine cavity, the IUD was successfully and completely removed. The patient did not require hospitalization or surgery, the procedure was virtually painless, and the surgery only took a few minutes. She was able to leave the hospital immediately afterward.
Case Study: Ms. Liu, 60 years old, had been menopausal for over 10 years. She had an IUD inserted in her uterus for contraception when she was younger. For the past two weeks, she had been experiencing lower abdominal discomfort and wanted to have the IUD removed. An examination revealed that her cervix had atrophied, and due to two previous cesarean sections, her uterus was tightly adhered to the anterior abdominal wall, making the cervix invisible. Without a visible cervix, removal was impossible! It was like not being able to find the door or enter the house. This greatly distressed Ms. Liu and her daughter. After discussion, the doctors determined that this problem could be solved with hysteroscopy! Under direct hysteroscopic visualization, the cervix was successfully located and the uterine cavity was accessed. It was discovered that the IUD was embedded in the uterine wall. With the assistance of hysteroscopy and ultrasound, the IUD was successfully removed in just 10 minutes, resolving Ms. Liu's major problem.
This procedure utilizes the natural vaginal cavity, achieving a scarless and incision-free outcome. Using hysteroscopic endoscopy, the intrauterine device (IUD) was successfully removed even when the cervix was severely atrophied and could not be exposed. It truly is a case of "a small hysteroscope solving a big problem!" We also want to remind all women that if you have been menopausal for six months, please remove your IUD as soon as possible. After menopause, the uterus shrinks, but the IUD size remains the same, greatly increasing the risk of IUD displacement or embedment!
Expert Interpretation: In fact, cases like Ms. Chen's and Aunt Liu's are not uncommon; medically, this is known as IUD displacement.
What are the causes of IUD displacement?
1. Improper operation that causes the IUD to be placed outside the uterine cavity;
2. The IUD is too large, too hard, or the uterine wall is thin and soft, causing the IUD to gradually displace outside the uterine cavity due to uterine contractions.
02. Diagnosis of IUD Displacement?
IUD displacement refers to a condition where an intrauterine device (IUD) is not in its normal position within the uterine cavity. This includes IUD displacement to the lower part of the uterus, embedding, and ectopic displacement.
1. A normal metallic IUD, as seen on a sonographic image, is a strong echo centered in the endometrial cavity, surrounded by a low-echo halo of endometrial tissue. Additionally, the distance between the upper edge of the IUD and the fundus of the uterus, or the distance between the lower edge of the IUD and the internal os of the uterus, can be used to determine if the IUD is in a normal position.
2. Grading of IUD Displacement: Mild: Upper edge of the IUD <25mm from the serosal surface of the fundus; Moderate: Upper edge of the IUD 25-35mm from the serosal surface of the fundus; Severe: Upper edge of the IUD >35mm from the serosal surface of the fundus.
3. IUD embedding depth in the uterine myometrium: Mild: IUD embedded in the myometrium less than 1/3; Moderate: Embedded in the myometrium less than 1/3 to 2/3; Severe: IUD embedded in the myometrium less than 2/3 or reaching the uterine serosa.
03 How to prevent IUD displacement?
First, choose a reputable medical institution for IUD insertion. Second, complete a thorough pre-operative examination to rule out genital malformations (such as septate uterus, double uterus, etc.), genital tumors (such as submucosal fibroids), and serious systemic diseases. Also, choose an appropriate IUD size and insert it 3-7 days after menstruation ends.
04. What precautions should be taken after IUD insertion?
1. Avoid heavy physical labor for one week after insertion.
2. Refrain from tub baths and sexual intercourse for one week after insertion.
3. Follow-up appointments are required at 1, 3, 6, and 12 months after the first year, and annually thereafter until discontinuation. Seek medical attention immediately for any special circumstances.
4. Remove the IUD promptly when it reaches its designated placement period.
05. Does an IUD always need to be removed?
First, it's important to know that IUDs have a limited lifespan. If they exceed this lifespan, it's recommended to remove them promptly, considering both contraceptive effectiveness and the risk of long-term complications.
For women within one year of menopause who no longer need contraception, the IUD should be removed promptly. After menopause, estrogen and progesterone levels drop significantly, the uterus shrinks, the cervix tightens, and the uterine muscle layer thins. Since the size of the IUD remains constant, the shrinking uterus may cause it to become embedded in the uterine wall, a condition known as IUD embedding. If it embeds in a blood vessel, it can cause severe bleeding; if it migrates into the abdominal cavity, it can cause a series of abdominal complications (abdominal pain, infection, etc.); if it migrates to the bladder and embeds in the bladder cavity, it may cause stones and unexplained hematuria (as in Ms. Wang's case of an ectopic IUD). Regardless of the type of displacement, removal can be difficult or unsuccessful, and may even require open surgery.
Older women are more prone to illness, and some illnesses require MRI scans, which are generally not possible with an IUD in place. Therefore, for women using IUDs, once they are inserted, they will need to be removed. Don't take chances and think that since you don't feel anything, you can leave it in your uterus. If you start experiencing symptoms later, it will likely require more extensive treatment.
Therefore, we would like to remind women of childbearing age and perimenopausal women to choose a reputable hospital to have the correct type of IUD inserted. IUDs have a limited lifespan, and should be removed promptly when they expire or when contraception is no longer needed.
Pre- and Post-operative Precautions for Hysteroscopy
Pre-operative:
1. Hysteroscopy is generally best performed 3-7 days after menstruation ends;
2. Sexual intercourse is prohibited for three days after menstruation or before the procedure;
3. Pre-operative examinations required: routine vaginal discharge test, complete blood count, coagulation function test, pre-operative four tests, liver and kidney function tests, blood type identification, and electrocardiogram.
Post-operative care:
1. Abstain from sexual activity and tub baths for one month post-surgery;
2. Rest for at least one week post-surgery;
3. Administer appropriate antibiotics post-surgery;
4. Seek immediate medical attention if vaginal bleeding occurs;
5. Collect the pathology report 7 days post-surgery.
- Recommended news
- 【General Surgery Laparoscopy】Cholecystectomy
- Surgery Steps of Hysteroscopy for Intrauterine Adhesion
- [ENT Surgery: Nasal Endoscopy] Endoscopic Treatment of Nasal Polyps
- [Otolaryngology Nasal Endoscopy] Methods and Precautions for Nasal Bleeding Control under Nasal Endoscopy
- [Orthopedic UBE Section] Four Years of Evolution of UBE Technology: From Lumbar Fusion to the "Forbidden Zone" of Thoracic and Cervical Spine, and the Unignorable "Hydraulic Pressure Crisis"