【Hysteroscopy】Removal of Intrauterine Foreign Body under Hysteroscope
Release time: 23 Mar 2021 Author:Shrek
Overview
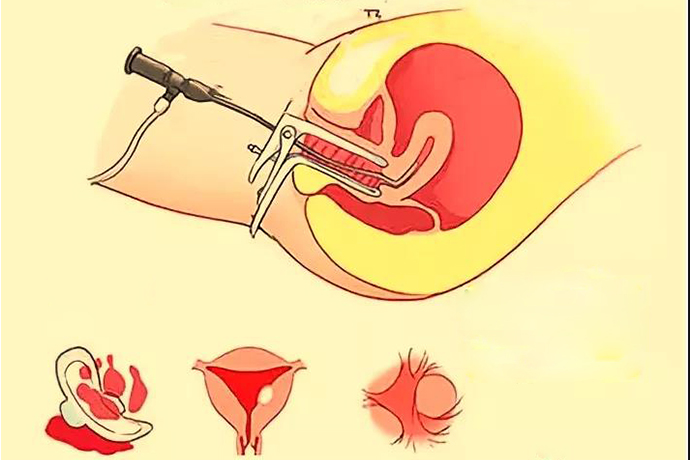
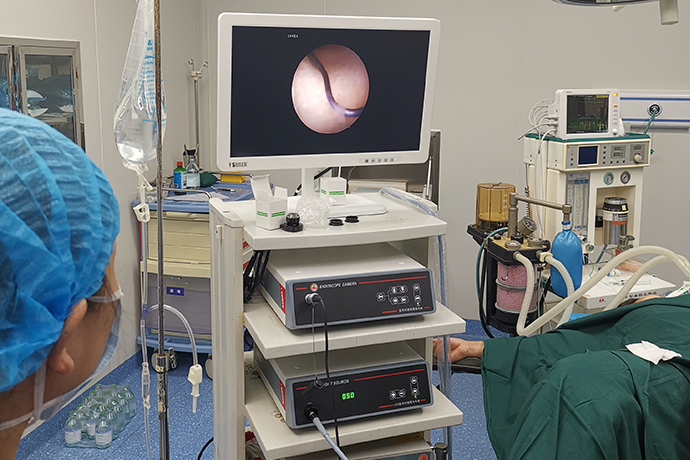
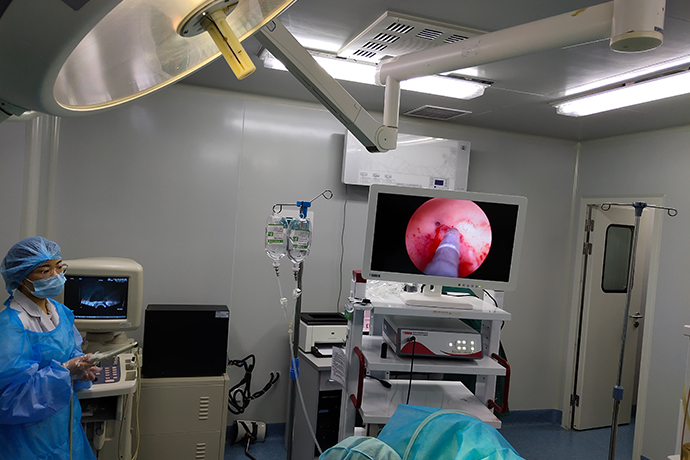
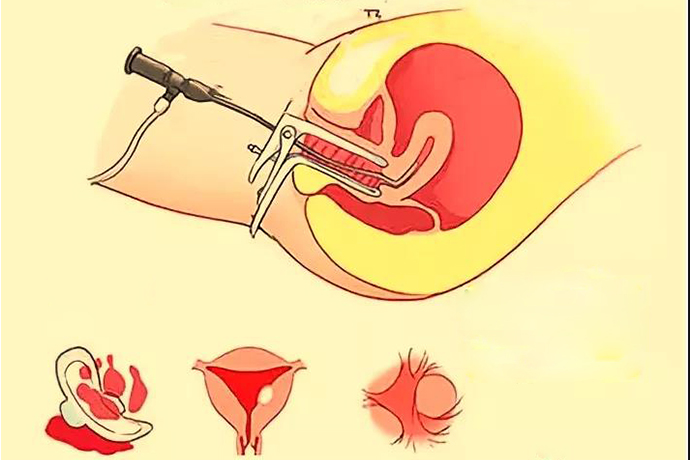
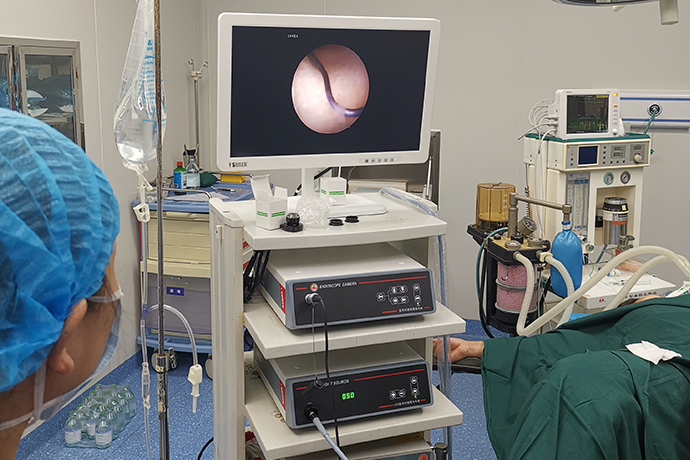
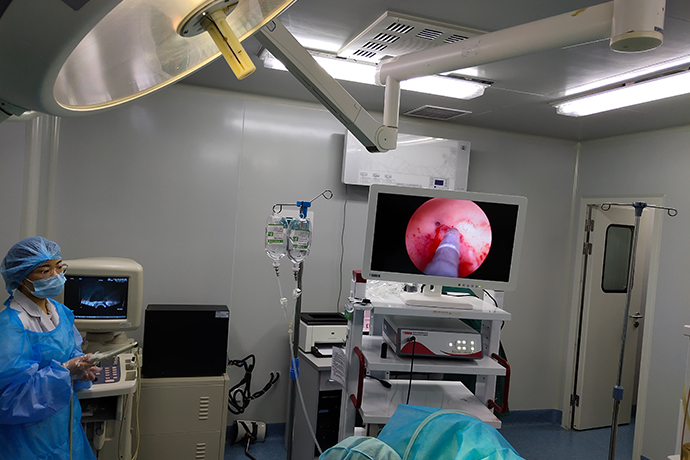
Hysteroscopy is a new, minimally invasive gynecological diagnosis and treatment technology, a kind of imaging light source endoscope used for intrauterine inspection and treatment, including hysteroscope, camera system, LED cold light source, irrigation pump and other instruments; It uses the front part of the endoscope body to enter the uterine cavity and has a magnifying effect on the observed part. It is intuitive and accurate as the preferred inspection method for gynecological bleeding diseases and intrauterine lesions.
The foreign body can be found directly under the hysteroscope, and the location can be accurately located. Removal of foreign bodies is safe, with a high success rate, and less trauma. If under the supervision of B-ultrasound, the operation is safer and more effective. To
The most common intrauterine foreign body is the fragment of the intrauterine contraceptive device, followed by the embryonic material and fetal bone remaining from abortion or mid-term labor induction, and rare cervical dilation rods, loop hooks, surgical sutures, etc. are rare. Diagnosis is not difficult, but due to factors such as small foreign body, uterine bleeding, endometrial fragments or intrauterine lesions, it may be difficult to remove the foreign body, and the foreign body needs to be removed under a hysteroscope.
Hysteroscopy Positioning Biopsy
Basic operation
(1) Hysteroscopy first. The hysteroscope is inserted into the uterine cavity through the vagina and cervical canal, and the shape, size, scope and texture of the lesion in the uterine cavity are checked under direct vision, and the location of the sample is determined.
(2) The hysteroscopic biopsy forceps are delivered to the uterine cavity along the operating channel of the hysteroscope, or placed into the uterine cavity along the gap between the mirror body and the cervical sidewall.
(3) Under direct vision of the hysteroscope, use the biopsy forceps to clamp the lesion tissue and pull it to separate it from the lesion. The biopsy forceps and the hysteroscope are simultaneously withdrawn from the uterine cavity, and the tissue specimen is taken out
(4) Repeat the above actions to ensure that the amount of tissue sample taken out is sufficient to send the case for examination.
(5) Insert the hysteroscope again to check the wound in the uterine cavity for active bleeding
Related Matters
(1) Intrauterine contraceptive device: The hysteroscope is equipped with foreign body forceps, etc., which can clamp the IUD under direct vision. If the strength is insufficient or incarcerated, a surgical hysteroscope is required. Use a ring electrode or a needle electrode to cut the surrounding muscle tissue and remove the remaining IUD. If the IUD is too deeply incarcerated, laparoscopy should be combined to determine whether the IUD has penetrated the serosal layer.
Symptoms: Difficulty in removing the device, broken IUD, ectopic
(3) Embryo and fetal bone residue: miscarriage, incomplete abortion, missed abortion, placental adhesions, placental implants, etc., can cause embryos and fetal bone to remain in the uterine cavity, causing irregular bleeding, intrauterine adhesion and stimulation Infertility and other conditions. Blind diagnostic curettage may not be able to scrape or scrape the remaining embryonic tissue. Hysteroscopy can make a clear diagnosis and remove residual uterine tissue, with clear positioning, safe, effective, and small bed. For those who are not incarcerated, they can be directly taken out with an electrosurgical loop or clamped by oval forceps under the supervision of B-ultrasound.
A summary of the techniques of hysteroscopic surgery
When the image is blurred after the lens is cast, it is recommended to withdraw the lens to the cervix to observe and judge the direction of the endoscope. Beginners often think that closer images will be clear, and it is possible to insert the uterine wall if you continue to move forward.
Keep in mind that 4 should and 1 shouldn’t
(1) should ask the patient to remove dandruff metal jewelry
(2) should check the electrode and energy output power
(3) should check the uterine dilatation fluid (20% mannitol is commonly used for unipolar resection)
(4) the statement that the patient needs should be monitored during the operation is boosted
(5) The operation time should not be too long, and the water should not be too much
Hysteroscopy is a new, minimally invasive gynecological diagnosis and treatment technology, a kind of imaging light source endoscope used for intrauterine inspection and treatment, including hysteroscope, camera system, LED cold light source, irrigation pump and other instruments; It uses the front part of the endoscope body to enter the uterine cavity and has a magnifying effect on the observed part. It is intuitive and accurate as the preferred inspection method for gynecological bleeding diseases and intrauterine lesions.
The foreign body can be found directly under the hysteroscope, and the location can be accurately located. Removal of foreign bodies is safe, with a high success rate, and less trauma. If under the supervision of B-ultrasound, the operation is safer and more effective. To
The most common intrauterine foreign body is the fragment of the intrauterine contraceptive device, followed by the embryonic material and fetal bone remaining from abortion or mid-term labor induction, and rare cervical dilation rods, loop hooks, surgical sutures, etc. are rare. Diagnosis is not difficult, but due to factors such as small foreign body, uterine bleeding, endometrial fragments or intrauterine lesions, it may be difficult to remove the foreign body, and the foreign body needs to be removed under a hysteroscope.
Hysteroscopy Positioning Biopsy
Basic operation
(1) Hysteroscopy first. The hysteroscope is inserted into the uterine cavity through the vagina and cervical canal, and the shape, size, scope and texture of the lesion in the uterine cavity are checked under direct vision, and the location of the sample is determined.
(2) The hysteroscopic biopsy forceps are delivered to the uterine cavity along the operating channel of the hysteroscope, or placed into the uterine cavity along the gap between the mirror body and the cervical sidewall.
(3) Under direct vision of the hysteroscope, use the biopsy forceps to clamp the lesion tissue and pull it to separate it from the lesion. The biopsy forceps and the hysteroscope are simultaneously withdrawn from the uterine cavity, and the tissue specimen is taken out
(4) Repeat the above actions to ensure that the amount of tissue sample taken out is sufficient to send the case for examination.
(5) Insert the hysteroscope again to check the wound in the uterine cavity for active bleeding
Related Matters
(1) Intrauterine contraceptive device: The hysteroscope is equipped with foreign body forceps, etc., which can clamp the IUD under direct vision. If the strength is insufficient or incarcerated, a surgical hysteroscope is required. Use a ring electrode or a needle electrode to cut the surrounding muscle tissue and remove the remaining IUD. If the IUD is too deeply incarcerated, laparoscopy should be combined to determine whether the IUD has penetrated the serosal layer.
Symptoms: Difficulty in removing the device, broken IUD, ectopic
(3) Embryo and fetal bone residue: miscarriage, incomplete abortion, missed abortion, placental adhesions, placental implants, etc., can cause embryos and fetal bone to remain in the uterine cavity, causing irregular bleeding, intrauterine adhesion and stimulation Infertility and other conditions. Blind diagnostic curettage may not be able to scrape or scrape the remaining embryonic tissue. Hysteroscopy can make a clear diagnosis and remove residual uterine tissue, with clear positioning, safe, effective, and small bed. For those who are not incarcerated, they can be directly taken out with an electrosurgical loop or clamped by oval forceps under the supervision of B-ultrasound.
A summary of the techniques of hysteroscopic surgery
When the image is blurred after the lens is cast, it is recommended to withdraw the lens to the cervix to observe and judge the direction of the endoscope. Beginners often think that closer images will be clear, and it is possible to insert the uterine wall if you continue to move forward.
Keep in mind that 4 should and 1 shouldn’t
(1) should ask the patient to remove dandruff metal jewelry
(2) should check the electrode and energy output power
(3) should check the uterine dilatation fluid (20% mannitol is commonly used for unipolar resection)
(4) the statement that the patient needs should be monitored during the operation is boosted
(5) The operation time should not be too long, and the water should not be too much
- Recommended news
- 【General Surgery Laparoscopy】Cholecystectomy
- Surgery Steps of Hysteroscopy for Intrauterine Adhesion
- [ENT Surgery: Nasal Endoscopy] Endoscopic Treatment of Nasal Polyps
- [Otolaryngology Nasal Endoscopy] Methods and Precautions for Nasal Bleeding Control under Nasal Endoscopy
- [Orthopedic UBE Section] Four Years of Evolution of UBE Technology: From Lumbar Fusion to the "Forbidden Zone" of Thoracic and Cervical Spine, and the Unignorable "Hydraulic Pressure Crisis"