【Hysteroscopy】Endometrial Polyps
Release time: 30 Mar 2021 Author:Shrek
Endometrial polyps are a common disease in gynecology. Many women are concerned about whether endometrial polyps will affect pregnancy. What is the existence of endometrial polyps?
We can think of the endometrium as ground, and fertilized eggs are equivalent to seeds, then polyps are equivalent to weeds! The growth of weeds on the ground may interfere with the growth and development of seeds. Of course, we must be urgent! With age, the incidence of endometrial polyps will gradually increase, but we should not worry too much.
Guidelines for identifying the presence of polyps
1. Increasing age is the most common risk factor for endometrial polyps (Grade B)
2. For women with endometrial polyps, abnormal uterine bleeding is the most common symptom (Grade B)
3. Infertile women are more likely to have endometrial polyps (Grade B).
4. The natural remission rate of endometrial polyps is as high as 25%, and small polyps are more likely to regress spontaneously (Grade A)
5. Drugs such as tamoxifen may induce the formation of endometrial polyps (Grade B). It is rare that aging causes the malignant transformation of polyps; abnormal uterine bleeding symptoms and the use of tamoxifen increase the possibility of polyps malignant transformation (Grade B).
Polyp diagnosis guide
1. Vaginal ultrasound provides reliable information for the detection of endometrial polyps, and the one that is suitable for application should be selected (Grade B).
2. Color or power Doppler improves the ability of vaginal ultrasound to diagnose endometrial polyps (Grade B).
3. The application of intrauterine contrast ultrasound (with or without 3D imaging) improves the diagnostic ability of endometrial polyps (Grade B).
4. Blind dilation, curettage or biopsy should not be used for the diagnosis of endometrial polyps (Grade B).
Polyp treatment guidelines
1. Especially for small, asymptomatic polyps, conservative treatment is reasonable (Grade A).
2. Drug treatment of polyps is not currently recommended (Grade B).
3. Hysteroscopic polypectomy is still the gold standard of treatment (Grade B).
4. There is no significant difference in the clinical prognosis of different hysteroscopic polypectomy (Grade C).
5. Symptomatic women after menopause should have polyps removed and histological evaluation (Grade B).
6. Hysteroscopic resection is better than hysterectomy, based on its minimally invasive, low cost and relatively low surgical risk (Grade C).
For infertile women suffering from polyps, surgical removal of polyps helps to conceive naturally or assisted by assisted reproductive technology for a greater chance of success (Grade A).
1. Why do you feel that many people around you have polyps? Is it related to genetics?
Endometrial polyps, in simple terms, are a common gynecological disease caused by the overgrowth of the uterine lining. The number can be simple or large, the diameter can be large or small, and it can be divided into sessile or pedicle. The incidence is about Between 7.8% and 34.9%. The 2015 AAGL guidelines pointed out that the high-risk factors for endometrial polyps include age, hypertension, obesity, and tamoxifen use.
Well, it has nothing to do with heredity.
2. Is there a relationship between endometrial polyps and estrogen?
Yes! Some people even go through a B-ultrasound when they are coming to menstruation, and they find that the smaller "polyps" may actually be thickened endometrium. When the menstruation is just clean, the B-ultrasound is gone. Because the endometrium is affected by estrogen and progesterone, it falls off regularly every month, which causes menstruation once a month.
Peng et al. studied the endometrial polyp tissue and the endometrial tissue surrounding the polyp in 53 cases of premenopausal women. The results showed that the expression of estrogen receptor in the endometrial polyp tissue was higher than that in the normal endometrial tissue. The estrogen receptors are high. In addition, Gul et al. studied 25 patients with premenopausal endometrial polyps and 25 patients with postmenopausal endometrial polyps, and found that the expression of estrogen and progesterone receptors in polyp glands of postmenopausal women was higher than that in the matrix.
3. What are the manifestations of polyps?
Polyps smaller than 1 cm are basically unfeeling. They were only discovered during the physical examination. When they grow up, they start to be demon... such as menstrual disorders, prolonged menstrual periods, inexhaustible menstruation, periovulation Period bleeding, etc.
4. Will polyps affect pregnancy?
Endometrial polyps are pedicled or sessile neoplasms that protrude into the uterine cavity, which changes the environment in the uterine cavity and is not conducive to the implantation of the embryo. It has been reported in the literature that the incidence of endometrial polyps in infertility patients is as high as 14.89%, and the older the age is, the risk of developing the disease increases. The pregnancy rate of infertility patients after endometrial polyp removal can be increased to 35%. ~35%.
5. Will polyps become malignant?
It is not easy for endometrial polyps to deteriorate. The incidence rate is usually 0% to 12.9%, and it depends on the study population. Most scholars believe that the risk of endometrial polyps malignant transformation increases with age, while the risk of polyps malignant transformation in premenopausal women seems to be very low. But with age, vaginal bleeding after menopause often indicates the possibility of malignant transformation.
6. Will polyps heal by themselves?
The natural remission rate of endometrial polyps is as high as 25%, and compared with polyps greater than 1 cm in length, smaller polyps are more likely to regress spontaneously.
7. What conditions need surgery?
Have clinical symptoms, such as irregular vaginal bleeding;
Postmenopausal polyps with bleeding need to be vigilant against malignant changes and should be actively treated;
Removal of polyps in infertile women can improve the ability of natural conception;
Removal of polyps before IVF can help the success rate of IVF.
At present, hysteroscopic polypectomy is the main treatment method, and the operation is safe, but blind curettage is not recommended. Surgery is usually performed 3 to 7 days after menstruation is clean.
8. Can patients with endometrial polyps take progesterone?
There is no clear evidence to support the use of progesterone to cause hormone withdrawal endometrial peeling and the use of an intrauterine progesterone sustained-release ring to treat endometrial polyps. The 2015 AAGL guidelines put forward: Drug therapy has limited effects on polyps, and drug therapy is not recommended. For large and symptomatic polyps, hysteroscopic resection is still the gold standard.
9. Why do endometrial polyps relapse after surgery?
The overall recurrence rate after surgery is about 2.5% to 3.7%, mainly because the cause of polyp formation has not gone, and the second is that the root of the polyp has not been cut clean.
10. How to treat if recurrence?
If it does not cause vaginal bleeding and does not affect pregnancy, it does not need to be treated, and there is no need to repeat the operation.
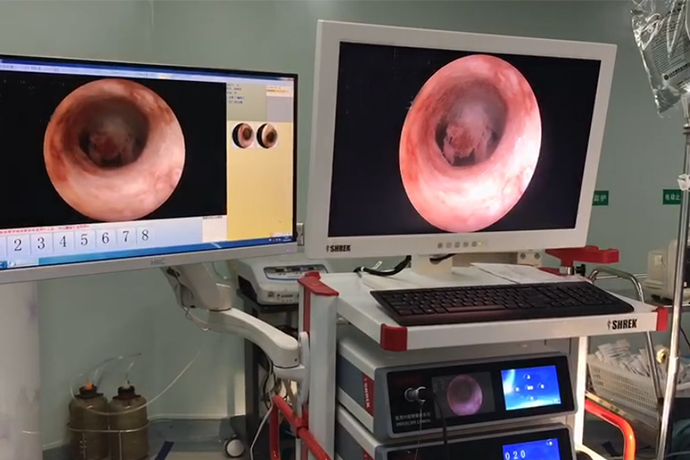
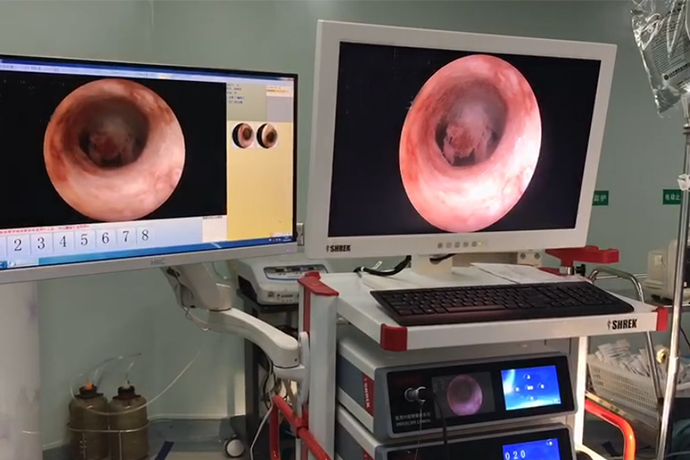
Hysteroscopy is currently the most widely used diagnostic method that can directly view the physiological and pathological changes of the endometrium, and is regarded as the gold standard for the diagnosis of endometrial diseases. Its advantages are: ① Looking directly at the uterine cavity, it can clarify the size, number, and location of polyps; ②The rate of missed diagnosis is low, and the condition of the polyp root and the endometrium around the polyp can be explored at the same time; ③The results of hysteroscopy and the final pathological examination results The coincidence rate is higher. However, hysteroscopy is an invasive operation, and there are risks of uterine perforation and massive bleeding. In addition, intraoperative pain increases the cardiovascular and cerebrovascular reactions, especially in older patients with severe medical diseases, which limits the application of hysteroscopy to a certain extent.
How to treat
01 expecting treatment
Functional endometrial polyps are derived from mature endometrium and can periodically change with the fluctuation of hormone levels in the body, especially polyps with a diameter of less than 1.0 cm, which can partly or completely fall off by themselves during menstrual cramps.
02 Curettage
Traditional curettage is performed under blind vision and is the main way to treat endometrial polyps. However, curettage is not easy to scrape the fundus and bilateral corners of the uterus, and may miss 1 /3 to 1 /4 of the uterine cavity area, the residual rate can be as high as 20% to 25%. Curettage is easy to damage the endometrium, which can easily lead to postoperative infection, intrauterine adhesions, and infertility.
03 Hysteroscopic polypectomy
The polyps can be removed from the pedicle under direct vision, and the damage to the normal endometrium is small. For patients with fertility requirements, the hysteroscopy operation will not have a negative impact on the physiological function of the ovary.
3.1 Hysteroscopic polypectomy
Polyp clamping and removal after hysteroscopic positioning is widely used because of its simple operation and operation time. However, it is difficult to remove the root of the internal polyp during the operation. The originally active part is prone to over-proliferation again, resulting in high postoperative recurrence rate, short recurrence interval.
3.2 Hysteroscopic polyp resection
Complete removal of polyps under hysteroscopy to prevent in situ recurrence of polyps. At the same time, abnormal endometrial biopsy around polyps can further determine the nature and scope of endometrial lesions. Related research has also proved that after hysteroscopic electrosurgical resection The recurrence rate is significantly lower than that of hysteroscopic polypectomy, and the operation can still be repeated after recurrence.
3.3 Hysteroscopic endometrial resection
Including endometrial resection, endometrial vaporization resection, and endometrial electrocoagulation. Endometrial resection is the removal of 2 to 3 mm of the functional layer, basal layer and muscular layer of the endometrium. Compared with cutting and coagulation electrodes, the vaporization electrode can not only remove larger polyps, but also avoid multiple interruptions during the operation. The depth of tissue vaporization can reach 3 to 4 mm, and the coagulation range of the tissue around the vaporization surface is 1 to 3 mm. For menopause It is not suitable for women with uterine atrophy and thinning of the endometrium. Endometrial electrocoagulation uses rolling ball electrodes to electrocoagulate and destroy the functional layer of the endometrium. In patients with postmenopausal and abnormal uterine bleeding, the diameter of endometrial polyps is greater than 1 cm, which increases the risk of endometrial cancer and precancerous lesions. Patients with corresponding symptoms should be vigilant. For perimenopausal women who are older, have obvious menstrual changes, have serious medical diseases, and cannot tolerate open surgery, intraoperative polyps are removed and a full-thickness endometrial resection is performed, which can completely remove polyps and surrounding suspicious endometrium, and retain the normal anatomy of the pelvic cavity.

We can think of the endometrium as ground, and fertilized eggs are equivalent to seeds, then polyps are equivalent to weeds! The growth of weeds on the ground may interfere with the growth and development of seeds. Of course, we must be urgent! With age, the incidence of endometrial polyps will gradually increase, but we should not worry too much.
Guidelines for identifying the presence of polyps
1. Increasing age is the most common risk factor for endometrial polyps (Grade B)
2. For women with endometrial polyps, abnormal uterine bleeding is the most common symptom (Grade B)
3. Infertile women are more likely to have endometrial polyps (Grade B).
4. The natural remission rate of endometrial polyps is as high as 25%, and small polyps are more likely to regress spontaneously (Grade A)
5. Drugs such as tamoxifen may induce the formation of endometrial polyps (Grade B). It is rare that aging causes the malignant transformation of polyps; abnormal uterine bleeding symptoms and the use of tamoxifen increase the possibility of polyps malignant transformation (Grade B).
Polyp diagnosis guide
1. Vaginal ultrasound provides reliable information for the detection of endometrial polyps, and the one that is suitable for application should be selected (Grade B).
2. Color or power Doppler improves the ability of vaginal ultrasound to diagnose endometrial polyps (Grade B).
3. The application of intrauterine contrast ultrasound (with or without 3D imaging) improves the diagnostic ability of endometrial polyps (Grade B).
4. Blind dilation, curettage or biopsy should not be used for the diagnosis of endometrial polyps (Grade B).
Polyp treatment guidelines
1. Especially for small, asymptomatic polyps, conservative treatment is reasonable (Grade A).
2. Drug treatment of polyps is not currently recommended (Grade B).
3. Hysteroscopic polypectomy is still the gold standard of treatment (Grade B).
4. There is no significant difference in the clinical prognosis of different hysteroscopic polypectomy (Grade C).
5. Symptomatic women after menopause should have polyps removed and histological evaluation (Grade B).
6. Hysteroscopic resection is better than hysterectomy, based on its minimally invasive, low cost and relatively low surgical risk (Grade C).
For infertile women suffering from polyps, surgical removal of polyps helps to conceive naturally or assisted by assisted reproductive technology for a greater chance of success (Grade A).
1. Why do you feel that many people around you have polyps? Is it related to genetics?
Endometrial polyps, in simple terms, are a common gynecological disease caused by the overgrowth of the uterine lining. The number can be simple or large, the diameter can be large or small, and it can be divided into sessile or pedicle. The incidence is about Between 7.8% and 34.9%. The 2015 AAGL guidelines pointed out that the high-risk factors for endometrial polyps include age, hypertension, obesity, and tamoxifen use.
Well, it has nothing to do with heredity.
2. Is there a relationship between endometrial polyps and estrogen?
Yes! Some people even go through a B-ultrasound when they are coming to menstruation, and they find that the smaller "polyps" may actually be thickened endometrium. When the menstruation is just clean, the B-ultrasound is gone. Because the endometrium is affected by estrogen and progesterone, it falls off regularly every month, which causes menstruation once a month.
Peng et al. studied the endometrial polyp tissue and the endometrial tissue surrounding the polyp in 53 cases of premenopausal women. The results showed that the expression of estrogen receptor in the endometrial polyp tissue was higher than that in the normal endometrial tissue. The estrogen receptors are high. In addition, Gul et al. studied 25 patients with premenopausal endometrial polyps and 25 patients with postmenopausal endometrial polyps, and found that the expression of estrogen and progesterone receptors in polyp glands of postmenopausal women was higher than that in the matrix.
3. What are the manifestations of polyps?
Polyps smaller than 1 cm are basically unfeeling. They were only discovered during the physical examination. When they grow up, they start to be demon... such as menstrual disorders, prolonged menstrual periods, inexhaustible menstruation, periovulation Period bleeding, etc.
4. Will polyps affect pregnancy?
Endometrial polyps are pedicled or sessile neoplasms that protrude into the uterine cavity, which changes the environment in the uterine cavity and is not conducive to the implantation of the embryo. It has been reported in the literature that the incidence of endometrial polyps in infertility patients is as high as 14.89%, and the older the age is, the risk of developing the disease increases. The pregnancy rate of infertility patients after endometrial polyp removal can be increased to 35%. ~35%.
5. Will polyps become malignant?
It is not easy for endometrial polyps to deteriorate. The incidence rate is usually 0% to 12.9%, and it depends on the study population. Most scholars believe that the risk of endometrial polyps malignant transformation increases with age, while the risk of polyps malignant transformation in premenopausal women seems to be very low. But with age, vaginal bleeding after menopause often indicates the possibility of malignant transformation.
6. Will polyps heal by themselves?
The natural remission rate of endometrial polyps is as high as 25%, and compared with polyps greater than 1 cm in length, smaller polyps are more likely to regress spontaneously.
7. What conditions need surgery?
Have clinical symptoms, such as irregular vaginal bleeding;
Postmenopausal polyps with bleeding need to be vigilant against malignant changes and should be actively treated;
Removal of polyps in infertile women can improve the ability of natural conception;
Removal of polyps before IVF can help the success rate of IVF.
At present, hysteroscopic polypectomy is the main treatment method, and the operation is safe, but blind curettage is not recommended. Surgery is usually performed 3 to 7 days after menstruation is clean.
8. Can patients with endometrial polyps take progesterone?
There is no clear evidence to support the use of progesterone to cause hormone withdrawal endometrial peeling and the use of an intrauterine progesterone sustained-release ring to treat endometrial polyps. The 2015 AAGL guidelines put forward: Drug therapy has limited effects on polyps, and drug therapy is not recommended. For large and symptomatic polyps, hysteroscopic resection is still the gold standard.
9. Why do endometrial polyps relapse after surgery?
The overall recurrence rate after surgery is about 2.5% to 3.7%, mainly because the cause of polyp formation has not gone, and the second is that the root of the polyp has not been cut clean.
10. How to treat if recurrence?
If it does not cause vaginal bleeding and does not affect pregnancy, it does not need to be treated, and there is no need to repeat the operation.
Hysteroscopy is currently the most widely used diagnostic method that can directly view the physiological and pathological changes of the endometrium, and is regarded as the gold standard for the diagnosis of endometrial diseases. Its advantages are: ① Looking directly at the uterine cavity, it can clarify the size, number, and location of polyps; ②The rate of missed diagnosis is low, and the condition of the polyp root and the endometrium around the polyp can be explored at the same time; ③The results of hysteroscopy and the final pathological examination results The coincidence rate is higher. However, hysteroscopy is an invasive operation, and there are risks of uterine perforation and massive bleeding. In addition, intraoperative pain increases the cardiovascular and cerebrovascular reactions, especially in older patients with severe medical diseases, which limits the application of hysteroscopy to a certain extent.
How to treat
01 expecting treatment
Functional endometrial polyps are derived from mature endometrium and can periodically change with the fluctuation of hormone levels in the body, especially polyps with a diameter of less than 1.0 cm, which can partly or completely fall off by themselves during menstrual cramps.
02 Curettage
Traditional curettage is performed under blind vision and is the main way to treat endometrial polyps. However, curettage is not easy to scrape the fundus and bilateral corners of the uterus, and may miss 1 /3 to 1 /4 of the uterine cavity area, the residual rate can be as high as 20% to 25%. Curettage is easy to damage the endometrium, which can easily lead to postoperative infection, intrauterine adhesions, and infertility.
03 Hysteroscopic polypectomy
The polyps can be removed from the pedicle under direct vision, and the damage to the normal endometrium is small. For patients with fertility requirements, the hysteroscopy operation will not have a negative impact on the physiological function of the ovary.
3.1 Hysteroscopic polypectomy
Polyp clamping and removal after hysteroscopic positioning is widely used because of its simple operation and operation time. However, it is difficult to remove the root of the internal polyp during the operation. The originally active part is prone to over-proliferation again, resulting in high postoperative recurrence rate, short recurrence interval.
3.2 Hysteroscopic polyp resection
Complete removal of polyps under hysteroscopy to prevent in situ recurrence of polyps. At the same time, abnormal endometrial biopsy around polyps can further determine the nature and scope of endometrial lesions. Related research has also proved that after hysteroscopic electrosurgical resection The recurrence rate is significantly lower than that of hysteroscopic polypectomy, and the operation can still be repeated after recurrence.
3.3 Hysteroscopic endometrial resection
Including endometrial resection, endometrial vaporization resection, and endometrial electrocoagulation. Endometrial resection is the removal of 2 to 3 mm of the functional layer, basal layer and muscular layer of the endometrium. Compared with cutting and coagulation electrodes, the vaporization electrode can not only remove larger polyps, but also avoid multiple interruptions during the operation. The depth of tissue vaporization can reach 3 to 4 mm, and the coagulation range of the tissue around the vaporization surface is 1 to 3 mm. For menopause It is not suitable for women with uterine atrophy and thinning of the endometrium. Endometrial electrocoagulation uses rolling ball electrodes to electrocoagulate and destroy the functional layer of the endometrium. In patients with postmenopausal and abnormal uterine bleeding, the diameter of endometrial polyps is greater than 1 cm, which increases the risk of endometrial cancer and precancerous lesions. Patients with corresponding symptoms should be vigilant. For perimenopausal women who are older, have obvious menstrual changes, have serious medical diseases, and cannot tolerate open surgery, intraoperative polyps are removed and a full-thickness endometrial resection is performed, which can completely remove polyps and surrounding suspicious endometrium, and retain the normal anatomy of the pelvic cavity.

- Recommended news
- 【General Surgery Laparoscopy】Cholecystectomy
- Surgery Steps of Hysteroscopy for Intrauterine Adhesion
- [ENT Surgery: Nasal Endoscopy] Endoscopic Treatment of Nasal Polyps
- [Otolaryngology Nasal Endoscopy] Methods and Precautions for Nasal Bleeding Control under Nasal Endoscopy
- [Orthopedic UBE Section] Four Years of Evolution of UBE Technology: From Lumbar Fusion to the "Forbidden Zone" of Thoracic and Cervical Spine, and the Unignorable "Hydraulic Pressure Crisis"