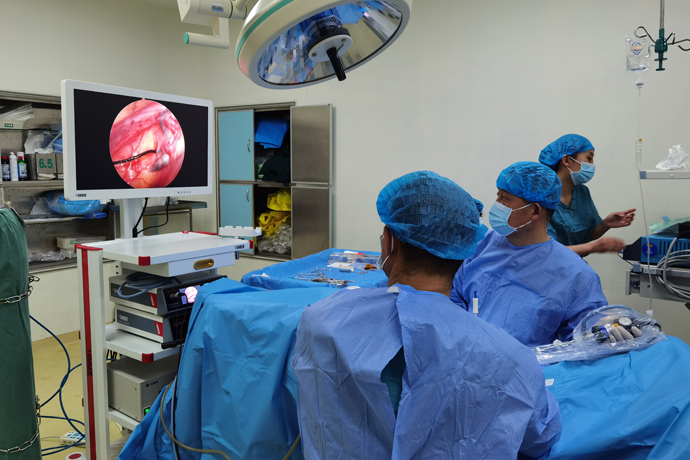
[General Surgery Laparoscopy] Laparoscopic retrorectal suspension patch fixation
Release time: 28 Oct 2025 Author:Shrek
Rectal prolapse (RP) refers to the downward displacement of the anal canal, rectum, and even the lower end of the sigmoid colon, protruding outside the anus, accompanied by pelvic floor dysfunction. Although a benign condition, RP can cause discomfort, mucus leakage, bleeding, and associated fecal incontinence or constipation, all of which can severely impact patients' quality of life. The incidence rate in women over 50 years of age is six times that of men. Although RP is generally associated with childbirth, nearly one-third of women with RP have no history of childbirth. Approximately 50% to 75% of patients with RP experience anal incontinence, and 25% to 50% experience constipation. Half of patients have pudendal neuropathy, which may contribute to the denervation and atrophy of the external anal sphincter.
There are detailed classifications of external rectal prolapse in China, including:
Grade I prolapse is approximately 3 cm long during defecation and retracts spontaneously after defecation. Grade II prolapse is the full-thickness protrusion of the rectum during defecation, measuring 4 to 8 cm and requiring manual pressure to reposition. Grade III prolapse is the protrusion of the anal canal, rectum, and part of the sigmoid colon, measuring over 8 cm, during defecation and is more difficult to reposition.
Grade I prolapse can be treated conservatively with traditional Chinese medicine, biofeedback, and injection therapy; Grade II prolapse can be treated with transanal surgery; and Grade III prolapse is primarily treated with transabdominal surgery. The goal of surgical treatment is to cure the anatomic abnormality and improve associated symptoms such as fecal incontinence, constipation, and pain. Rectal prolapse is a condition in which the rectum protrudes beyond the anus and is often associated with anatomical abnormalities such as lax levator ani muscles, a deep Douglas pouch, a redundant sigmoid colon, a cavernous anal sphincter, and loss or weakening of the sacrorectal fixation.
The advantages of laparoscopic retrorectal suspension mesh fixation are:
1. Adhering to the principle of preserving pelvic autonomic nerve function (PANP) during laparoscopic radical rectal cancer resection, this procedure maximizes pelvic autonomic nerve function under direct visualization, particularly preserving the neurovascular bundles (NVB) on both sides of the anterior wall, thereby protecting the patient's urinary and sexual function.
2. Laparoscopic suturing of the mesh to the sacral promontory, suturing the mesh to the bilateral "peritoneal wings," and circumferential suturing to eliminate the rectovesical pouch and elevate and reconstruct the pelvic floor ensure a low postoperative recurrence rate.
3. The procedure is performed entirely laparoscopically, requiring fewer and smaller abdominal incisions, resulting in minimal postoperative pain, excellent cosmetic results, and few complications, all contributing to high patient acceptance.
Surgical steps
Establishing the operating platform
After successful general anesthesia, the lithotomy position was adopted, and the surgical field was routinely disinfected and draped.
1. Make a circumbilical incision approximately 1.2 cm long in the supraumbilical skin fold, advancing the abdomen layer by layer. A 12mm trocar is inserted through this incision to establish pneumoperitoneum and maintain air pressure at 13-15 mmHg. A 30° laparoscopic lens is inserted through this trocar.
2. Under laparoscopic monitoring, avoid the inferior epigastric artery and insert a 5mm trocar at the line connecting the right lateral rectus abdominis muscle and the horizontal line of the umbilicus. This serves as a secondary access port for the primary surgeon.
3. Insert a 12mm trocar at the right McBurney point as the primary access port for the primary surgeon.
4. Insert a 5mm trocar at the intersection of the line connecting the left lateral rectus abdominis muscle and the horizontal line of the umbilicus. This serves as the primary access port for the assistant surgeon.
5. Insert a 5mm trocar at the left anti-McBurney point as the secondary access port for the assistant surgeon.
Exploration
The liver, gallbladder, stomach, duodenum, jejunum, cecum, ascending colon, transverse colon, and descending colon were normal. The inherent adhesion band between the distal lateral edge of the first curvature of the sigmoid colon and the left abdominal wall was absent, and no intersigmoid recess was observed. The intraoperative diagnosis was consistent with the preoperative diagnosis, and the decision was made to proceed with a 4K laparoscopic retrorectal suspension with patch fixation.
Surgical steps
Mobilization of the inner side of the left colon:
(1) Open the midline side of the sigmoid colon mesocolon: Use the intestinal forceps to grasp the rectum and pull it ventrally to tighten the sigmoid colon mesocolon. Use the sacral promontory as the entry point and the "yellow-white junction line" as a guide to open the sigmoid colon mesocolon from the caudal to the cranial side to the root of the small intestinal mesocolon. Then turn left and a loose gap will be seen. This is the fusion fascial gap (Toldt's gap) between the left mesocolon and the prerenal fascia. (2) Expand the Toldt's gap: The assistant's intestinal forceps continue to pull the upper rectum ventrally. The right intestinal forceps grasp the pedicle of the inferior mesenteric artery and hold it ventrally while maintaining tension. The surgeon carefully expands the Toldt's gap: Within this gap, expand the surgical plane to the left to reach the Toldt line where the sigmoid colon mesocolon disappears. Care was taken to maintain the integrity of the left colon mesentery and prerenal fascia, and to retain a layer of transparent prerenal fascia in front of the main iliac vessels. Through this fascia, the left ureter and genital vessels at the posterolateral level of the root of the sigmoid colon mesentery were visible (without causing damage to the inferior mesenteric plexus, left ureter, or left genital vessels). The range of dissection extended from the center to the left to the left paracolic gutter lateral to the genital vessels, and from the caudal to the cephalad side to the root of the inferior mesenteric artery.
Posterolateral Mobilization of the Left Hemicolon: The sigmoid mesocolon is retracted to the right. Starting from the intrinsic adhesion between the distal lateral edge of the first curvature of the sigmoid colon and the left abdominal wall, the left paracolic peritoneal fold is incised cephalad along the yellow-white junction (Toldt's line). The sigmoid colon is flipped to the right and mobilized to the right through the Toldt's space between the mesentery and the prerenal fascia, taking care to protect the left ureter and left genital vessels behind the prerenal fascia. The lateral sigmoid colon is completely penetrated in the midline plane and extended superiorly to the level of the lower sigmoid colon, taking care to protect the integrity of the prerenal fascia, sigmoid mesocolon, and native descending colon mesocolon.
Perirectal mobilization: Starting from the level of the sacral promontory, in the loose connective tissue space behind the upper rectal mesosome, the surgical plane is sharply extended posteriorly and laterally to the retrorectal space, until it reaches the supra-levator ani space.
(1) Posteriorly: Starting from the level of the sacral promontory, close to the colorectal mesosome, the surgical plane is extended caudally in the retrorectal space between the colorectal mesosome and the presacral fascia, the rectosacral fascia is cut, and the supra-levator ani space is entered and close to the levator ani muscle.
(2) (2) Laterally: The retrorectal space is extended to both sides, and the posterior space is used as a guide to free the perirectal space to both sides until it reaches the level of the supra-levator ani space. The inferior mesenteric artery and the superior rectal artery are not cut, the rectal lateral ligament is not severed, and the peritoneal reflection in front of the rectum is not opened. During the whole process, attention is paid to protecting the integrity of the pelvic autonomic nerves.
Retrorectal sling fixation:
Select a hernia mesh (material: polypropylene), trim it to a suitable shape, and place it behind the rectum in the abdominal cavity. Ensure that the mesh is fully unfolded and lies flat in the space behind the rectum.
After assisting with rectal elevation and correcting the prolapse, the upper segment of the mesh was secured to the anterior sacrococcygeal fascia with absorbable sutures (IMPORTANT: Secure securely! Looseness is not permitted). The mesh was embedded, and hemostasis was performed carefully to prevent postoperative pelvic floor infection. On the left side of the rectum, a continuous suture of 3-0 absorbable Vicryl was used to wrap and embed the left lateral peritoneum, the mesh, and the left fascia proper of the rectum, preventing the mesh from contacting the rectal surface. This allowed for complete peritonealization of the left lateral rectum (to prevent adhesion of the small intestine to the mesh). The same procedure was followed for the right side.
Finally, the left lateral seromuscular layer of the sigmoid colon was sutured to the left lateral peritoneum, suspending the sigmoid colon to the lateral abdominal wall.
Postoperative examination: Clean the surgical field, repeatedly flush the abdominal cavity with saline, and aspirate thoroughly. Check for active intraperitoneal bleeding. Reposition the bowel, count the instruments, align the gauze, and inspect the puncture sites for bleeding. Insert a No. 26 chest tube through the right lower quadrant operative port to the pelvic floor and secure it. Remove the laparoscope and puncture cannulas, suture each operative port layer by layer, and cover with a small dressing.

- Recommended news
- 【General Surgery Laparoscopy】Cholecystectomy
- Surgery Steps of Hysteroscopy for Intrauterine Adhesion
- [ENT Surgery: Nasal Endoscopy] Endoscopic Treatment of Nasal Polyps
- [Otolaryngology Nasal Endoscopy] Methods and Precautions for Nasal Bleeding Control under Nasal Endoscopy
- [Orthopedic UBE Section] Four Years of Evolution of UBE Technology: From Lumbar Fusion to the "Forbidden Zone" of Thoracic and Cervical Spine, and the Unignorable "Hydraulic Pressure Crisis"