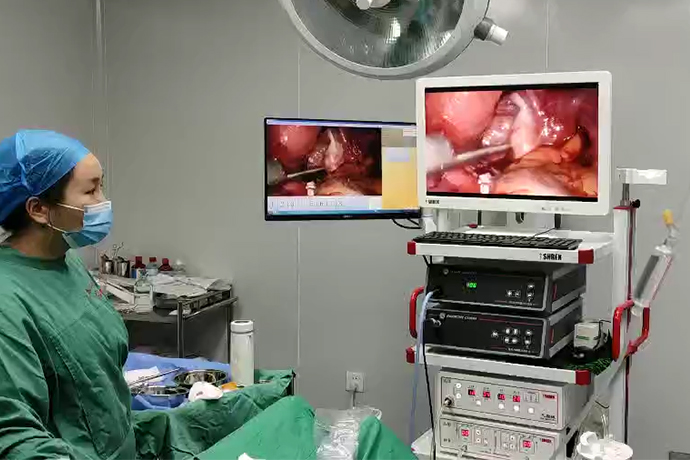
[Gynecological Laparoscopy] 4K laparoscopic pelvic and para-aortic lymph node dissection
Release time: 23 Aug 2023 Author:Shrek
Pelvic lymph node dissection, also known as pelvic lymph node dissection, is an important part of the surgical treatment of gynecological malignancies such as cervical cancer, endometrial cancer, ovarian cancer, and fallopian tube cancer. It is related to the surgical staging of patients and provides a basis for postoperative follow-up treatment.

Pelvic lymph node dissection is a common treatment for gynecological tumors. Lymph node dissection usually refers to the resection of the terminal common iliac artery and its surface lymphatic adipose tissue. Lymphatic adipose tissue of nostrils and nostrils were resected in sections.
Laparoscopic Pelvic Lymphadenectomy Technique
Pelvic lymphadenectomy should result in representative lymphadenectomy reflecting uterine lymphatic drainage. This includes the lymphatic axis of the external iliac vessels, as well as those of the fossa ellipse, the internal iliac vessels, and the common iliac arteries. Interestingly, the literature investigating patterns of lymphatic spread in these different regions is almost non-existent.
Although sentinel lymphadenectomy for endometrial cancer is incomplete and standardization for cervical cancer is not yet adequate, extensive research surrounding the identification of pelvic sentinel lymph nodes points to fairly stable lymph nodes located at the bifurcation of the common iliac artery and the internal and external iliac arteries. Appearance of the obturator nerve as it enters the ophthalmic socket medially.
Below is an overview of the method followed by a detailed explanation of the rationale.
1. Anatomical normalization - cephalad dissection of the ileocecum and resolution of pelvic sigmoid adhesions
2. Severing the round ligament to open the side wall of the pelvis
3. The caudal and medial sides of the peritoneal incision are short stretched toward the bladder
4. The peritoneal incision is extended and arc-shaped, passing through the external iliac vessels and opening the psoas muscle gap
5. The infundibulum ligament is centered and the ureter is exposed as it crosses the pelvic rim
6. Follow and cut the ureter into the renal pelvis
7. Separation of the ureter from the internal iliac artery
8. Moving to the front of our dissection again: separation of the umbilical ligament
9. Opening of the paravesical space
10. Opening the Obturator Fossa - Dissecting the Obturator Nerve
11. Complete lateralization of the internal iliac artery-umbilical artery/lateral umbilical ligament axis. Locating and dissecting this axis is critical because it allows us to do the most important thing gynecologists do in the pelvic sidewall: find where the uterine artery branches off from the internal iliac artery
12. Managing the arterial axis can often appear daunting to the uninitiated; however, aortic vascular injury is actually very rare. Literally pierce these large vessels directly. It is easy to perform blunt dissection on top of these arteries. NOTE: Ventrally, laterally, and even medially (up to the uterine artery branch), there are no obvious structures that leave the axis of the artery and thus serve as a safe "prep". The fact that the more fragile internal iliac veins are "protected" behind the arteries on both sides is not dangerous unless you expose more than half the circumference of the arteries
13. Exposure of uterine artery branch leaving internal iliac artery
14. Opening of the pararectal space
15. Begin lymphadenectomy from the most distal part of the external iliac artery. Distal: The circumflex vein crosses. This vein does not require coagulation and is of no importance. It often appears as a flattened ligamentous structure across the artery due to venous depression. To us, this means the distal end of the lymphadenectomy is "far enough"
16. Avoid interfering with the lateral psoas adipose tissue
17. Exposure of the external iliac artery, retrograde lymph node resection, using a combination of blunt (80%) and sharp (20%) methods
18. Try dismantling the whole
19. Distal, exposure of the internal iliac vein
20. Find the pelvis directly "below" that is, medial and dorsal to the internal iliac vein
21. Re-exposure of the obturator nerve
22. Begin to remove obturator lymph nodes
23. Separate the external iliac vessels from the psoas major and expose the obturator fossa from the side
24. Guided by the obturator nerve, further resect the obturator fossa lymph nodes
25. Continue to the internal iliac artery lymph node dissection
26. Remove the fork node (sentinel section)
27. Cut the remaining lymph node attachments into the obturator fossa and umbilical ligament
28. Expose the branches of internal iliac vein and common iliac vein
29. Removal of remaining and most proximal external iliac lymph nodes into en bloc resection tissue
30. Remove lymph nodes with inner bag as much as possible
31. The lymph node pad lateral to the common iliac artery (right side) was removed, completing the lymphadenectomy.
Below is a more detailed explanation of the above step-by-step method.
Finally, lymph node removal requires adequate lateral and craniofacial exposure. If the adhesions pulling the right ileocecum or left sigmoid toward the pelvis postoperatively are not initially removed, they must be done later, which is made more difficult because the planes are no longer anatomically original.
In particular, the physiological adhesions of the sigmoid colon to the left pelvic wall are very different. Getting them off takes a certain amount of practice. Opening of the retroperitoneum should be avoided at this time. Perfect dissection requires only sharp scissors. Excessive bleeding means that the anatomical plan is incorrect. Coagulation with electrocautery carries a high risk of febrile bowel injury.
Classic step. Should be open in the outermost position. Normally, there are no vessels associated with the round ligament, although in the British literature a variable so-called "Sim's artery" is often mentioned. Using a laparoscope means opening the retroperitoneum for immediate access to carbon dioxide, causing the artificial space to expand.
A short extension of the peritoneal incision caudally and medial to the bladder.
It is tempting to go further to the bladder, especially if the hysterectomy is part of the procedure; however, there is always a danger of running bleeding or even damaging the bladder.
The peritoneal incision is extended in an arc, traversing the external iliac vessels and opening the psoas space.
This is a critical step in the beginning of the operation. It is very safe to limit the incision to the peritoneal layer. The psoas space is one of the "safe" areas. The only danger is crossing the external iliac vessels, which could theoretically cause injury. Once the psoas space is reached, the incision is now curved upward, as far upward as possible. At this point, previous careful dissection and resection of the ileocecum on the right and the sigmoid on the left become critical. Every additional centimeter of the headrest helps in the next step: mobilization of the medial infundibulum ligament.
The infundibulum ligament is centered and the ureter is exposed as it crosses the pelvic rim
This step exposes the ureter. Dissection of the funnel-pelvic ligament always requires great care. In addition to tearing the ovarian veins (which takes some force...), there are many smaller blood vessels that can tear and cause unnecessary bleeding. This step needs to be done more than once, bluntly and carefully exposing the ureter. The right side is easier (no sigmoid).
Follow and cut the ureter into the renal pelvis.
This can be very easy (no surgery, no adhesions) or very difficult when the tissue does not yield easily. Small peritoneal hemorrhages can be annoying and vague. Ideally, the ureter is easily trailed and, as it approaches the lateral pelvic wall, leads to the internal iliac artery, while the ureter extends medial to the rectouterine space in the peritoneum. There are subtle differences in the position of the ureters, but they are oddly difficult to describe. On the right, the ureter is "top" and medial to the internal iliac artery, while on the left, it is even more arterial at the pelvic rim.
If this step is too difficult, focus on the anterior part of the dissection first.
Separation of the ureter from the internal iliac artery
This will cause branching of the uterine arteries. At the same time, it is prepared to enter the para-rectal space (which only needs to be opened if a radical hysterectomy is planned).
Moving to the front of our anatomy again: separation of the lateral umbilical ligament
This step can be performed at any time. In general, the most important rule of the "Rules of Anatomy" is: Every surgical step is different. There's no point in sticking with particularly difficult parts when other areas can be handled more easily. Often, miraculously, when going back to the difficult area, the anatomy becomes friendlier and the procedure can move forward, which was very difficult before. No matter how difficult the dissection or how obese the patient is, the lateral umbilical ligament can usually be found on the anterior abdominal wall and then emerges in a cephalad retrograde fashion for positioning in the most desperate pelvis.
The paravesical space, just medial to the lateral umbilical ligament, is the most accessible space of the pelvis. It should be straightforward to dissect. Dissection can be performed almost to the pelvic floor, where unnecessary bleeding occurs, so the last centimeter is still unnecessary and should be avoided. In thin patients, dissection of the paravesical space sometimes leads laterally to the obturator nerve and posterior to the ureter.
Obturator fossa open-obturator neurotomy
Medial to the lateral umbilical ligament (including the occluded umbilical artery), which can enter the obturator fossa. This sometimes requires some sharp dissection because the lateral umbilical ligament can be very lateral, almost attached to the adjacent structure, the external iliac vein. Therefore, safe opening of this space should be performed directly lateral to the lateral umbilical ligament, as far as possible from the lateral pelvic wall. The "bottom" of the obturator fossa is the obturator nerve, which needs to be freed from the surrounding fat and lymphatic tissue at some distance in order to be truly visible for the rest of the procedure. The obturator nerve requires frequent checking of its position. It follows the age-old rule of the ureter: "now you see, now you can't" and is easily injured by cauterization, thermal energy, or sharp transections. The obturator nerve is the largest nerve structure in the pelvis. It is accompanied by obturator vessels that rarely require coagulation but, if not respected, may cause unnecessary and annoying bleeding. The obturator vein often branches off from the external iliac vein, in which case coagulation is recommended to facilitate lymphadenectomy.
Complete lateralization of the internal iliac artery-umbilical artery/lateral umbilical ligament axis
After successful caudal and cephalad approaches, this axis is often connected to the lateral pelvic wall. However, there are no important vessels or other structures other than small peritoneal vessels, so sharp dissection should bring the most dorsal part of the surgical field to the vascular axis.
Branches of uterine artery detach from internal iliac artery
Locating where the uterine artery branches off from the internal iliac artery (at an almost 90° angle) remains the most critical skill for the gynecologist to master. It is essential for radical hysterectomy but very useful in many challenging gynecological procedures. Basically, it requires adequate separation of the paravesical and pararectal spaces, which are separated by the uterine artery.
open pararectal space
Pelvic lymphadenectomy does not necessarily require opening the pararectal space, nor does isolation of the uterine artery. This is necessary as part of a radical hysterectomy.
Most distal internal iliac artery lymphadenectomy
Once all relevant structures have been delineated and all spaces have been opened, lymphadenectomy can safely begin. Atraumatic lymph node capture is usually possible. Lymph nodes bleed easily, so care needs to be taken. The guiding structure of the first segment is the external iliac artery.
Distal: The circumflex vein crosses, taking care not to enter too far into the inguinal canal. Exposure of this vein, crossing the external iliac artery is sufficient to reach the distal end of the anatomy.
Avoid interfering with the lateral psoas adipose tissue
Many surgeons feel that this nodal-free fad pad is too easy to remove, leading to an increased incidence of lymphoceles/lymphocysts. It certainly does not increase the number of lymph nodes.
The external iliac artery was exposed and lymph nodes were dissected retrogradely using a combination of blunt (80%) and sharp (20%) approaches.
The external iliac artery needs to be exposed and protected. However, this is a solid structure and the lymph nodes can be "pulled" out of the artery in a blunt fashion - this is done routinely in open cases.
Distal exposure of the internal iliac vein
After resection of the lymph nodes on the external iliac artery, the movement is medial, down to the very thin and often "empty" external iliac vein (due to the patient's head-down position).
The key is to identify the "lower" edge of the vein to ensure that the paper thin vessels are not accidentally injured. The danger is that an injured but "empty" external iliac vein may not bleed immediately.
Find the pelvis directly "below" that is, medial and dorsal to the internal iliac vein
This bony part of the pelvis is a key part of the anatomy. It allows safe access to the lateral limitation of the obturator space (obturator muscle) and further allows safe isolation of the obturator nerve.
Because the obturator lymphatic fat pad can be easily dissected from the smooth bone, it is also a good starting point for lymphadenectomy.
Lateral margin of knot resection: The psoas muscle is the most vulnerable to injury. The injury usually occurs just below the entry of the external iliac vein into the obturator fossa.
Crypt lymphadenectomy
When the external iliac vein is safely removed and the obturator nerve is visible, a lymphadenectomy is initiated rapidly, allowing the entering lymphatic vessels to be coagulated and severed, and then most of the lymph node tissue is directly removed. Abnormal obturator veins, branches of the external iliac vein require careful observation and usually must be coagulated and severed.
Separate the external iliac vessels from the psoas muscle and expose the obturator fossa laterally
For the laparoscopist, this step doesn't add much and doesn't need to be done at all costs. If the obturator perforator bleeds, it can be slightly better controlled. However, many traditional open surgeons firmly believe that this is an important part of pelvic lymphadenectomy, and they claim that the lymph nodes above the sacral nerve are a common site of recurrence, especially in cervical cancer, without conclusive evidence or empirically substantiated claims by the authors of this chapter .
Additionally, recent knowledge of uterine and cervical lymphatic drainage points to a common sentinel node in a completely different location.
Still, it's a nice and fairly easy trick to master. Sometimes, when all else fails, this may be the only way to find the obturator nerve.
Guided by the obturator nerve, further resection of the obturator fossa lymph nodes
In terms of mechanical force, a nerve is a fairly strong structure. However, the overlying attachments require careful dissection, taking care not to thermally damage the nerve.
Branches of external common iliac vein and internal iliac vein
The remaining lymph node attachments are cut into the obturator and lateral umbilical ligament with care. At this point, there is a tendency to pull the lymph node pack medially to make these attachments more visible. However, this can dangerously distort the course of the obturator nerve, and this must be borne in mind.
This is a good step in lymph node dissection. If you can actually see this branch, you must have completely removed the most relevant lymph nodes.
The remaining and most proximal external iliac artery lymph nodes are moved into en bloc resection tissue, and the lymphatic chain continuing to the common iliac artery must be severed at some point.
Lymph nodes are removed using the inner bag whenever possible.
Besides being more aesthetically pleasing, it also keeps your supra-syndromic trocar clean, which will be important for camera positioning there, during para-aortic lymph node dissection.
Lymphadenectomy is accomplished by removing the lymph node pads lateral to the common iliac artery (right). The lymph node tissue in this area is usually somewhat flat and patchy. Some bleeding is very common.
On the right, at a certain point, the posterior border becomes the inferior vena cava, which cannot be inadvertently injured.
Laparoscopic paraaortic lymphadenectomy technique
1. Positioning. Retrograde laparoscopy. 10mm port on the extra joint for the camera. The second assistant can only hold the camera. The surgeon looks at the head from the right side of the patient, and the first assistant looks at the head from the patient's left side.
2. Expose the pelvic rim - starting point is the common iliac artery.
3. Move the rectosigmoid to the left of the abdominal wall and the small intestine to the right of the abdominal wall. Adjust the head-down toe-height position as needed.
4. Lift the peritoneal covering over the right common iliac artery, creating an opening in the retroperitoneal space.
5. Using the truncus, the peritoneal incision is made upward toward the ligament of Treitz, avoiding all vulnerable structures.
6. In essence, preparation is the opening of the peritoneal tent required for surgery.
7. The tent needs to be extended to the right side of the patient, at this time the ureter needs to be separated from the right ovarian vein
8. The right ureter needs to be kept at a distance so that the psoas muscle space is directly exposed to the right side of the inferior vena cava.
9. When delineating the right edge of the vena cava, care must be taken to identify the branches of the ovarian vein and, if necessary, the vein needs to be coagulated.
10. Likewise, the intersection of the right ovarian arterioles needs to be identified to be respected or carefully coagulated and transected.
11. After fixing the "right side" of the tent, the left side needs to be determined.
12. First, the branches of the internal mesenteric artery need to be located. It is fairly constant midway between the aortic bifurcation and the crossing of the left renal vein, with a slight detachment on the left side of the aorta.
13. Finding the junction of the left renal vein was challenging. The dissection can't be sharp: cutting the inferior border of the left renal vein is a disaster that must never happen.
14. About 2 cm to the left of the aorta, the left ovarian vein begins to descend from the left renal vein. This corner is the most difficult part of the para-aortic lymphadenectomy
15. The tent is enough for now.
16. Lymphadenectomy can be performed from cranial to caudal or from caudal to skull. The decision on how to proceed is usually a case-by-case basis, depending on the individual anatomy. Distal dissections tend to be more difficult and risky, so should probably be the first step.
17. The preparation on the aorta is no problem; the inferior vena cava needs to be cut slowly and carefully. Even pulling on the lymphatic tissue can tear the venous hole that runs through the vein and can cause bleeding from the vena cava.
18. Bleeding from the vena cava requires immediate closure with pressure. About 90% of wounds can be stopped by applying sufficient pressure for at least 5 minutes. Portions that still bleed after prolonged compression need to be closed with 4-0 or 5-0 monofilament sutures.
19. Whole-body lymphadenectomy of the inferior vena cava and para-aortic space is challenging. We recommend a step-by-step approach in different spaces
20. Paraaortic area - inferior mesenteric artery (including the difficult angle between the left renal and left ovarian veins). 21. The para-aortic region below the inferior mesenteric artery (be careful, the ureter is very close to the left edge of the preparation and can be easily injured). Visualization of the left ureter remains a great challenge. The patient and mostly blunt dissection will eventually allow us to see this important structure. It is deeply embedded in the left adipose tissue and is not prone to blunt dissection, but it is dangerous to perform sharp dissection in this area.
22. Paracavity area, upper half - note the crossing of the right ovarian artery, branch of the right ovarian vein.
23. Paracavity area, lower half - note the perforating veins increasing in frequency towards the caudate area.
24. Interportal area - be careful not to injure the dorsal and descending lumbar veins.
25. Accessory vena cava area on the right side of the vena cava-psoas muscle space. Be careful not to damage the right ureter.
26. The key to paraaortic lymphadenectomy is to avoid major bleeding, as this usually requires laparotomy. 27. Lymph node tissue is usually small and can be removed through the umbilicus with a 10 mm trocar. Below is a more detailed explanation of the above step-by-step method.
Position. Retrograde laparoscopy. 10mm port on the extra joint for the camera. The second assistant can only hold the handle. The surgeon looks at the head from the right side of the patient, and the first assistant looks at the head from the patient's left side.
Of course, these are just suggestions. Every surgeon needs to figure out his or her best approach. Some surgeons may want to stand between the legs. However, readers are strongly encouraged to do so.
Expose the pelvic rim - starting point is the common iliac artery
It was also a test of the viability of this extremely challenging procedure. Without the ability to dissect the right common iliac artery, surgery would not be possible.
Move the rectosigmoid to the left side of the abdominal wall and the small bowel to the right side of the abdominal wall. Adjust the head-down toe-height position as needed.
At this point, we should discuss the order of surgery. From an oncological standpoint, it would be good to know if the pelvic lymph nodes are affected. In cervical cancer, this may be the reason for performing para-aortic lymph node dissection. However, given that para-aortic dissection is the most challenging part of the surgical procedure with the highest conversion rate (albeit still very low in the hands of skilled surgeons), one might consider starting with this part of the procedure. The advantage of this is that if the surgeon starts with a para-aortic dissection, the attachment of the sigmoid to the left pelvic sidewall has not been removed, facilitating lateralization.
The retroperitoneal space can be opened by lifting the peritoneal covering over the right common iliac artery
Most laparoscopic tumor surgeries can be done with the help of first assistants. However, paraaortic dissection is different. At least one minimum-skilled assistant must be present.
Utilizing the truncus, the peritoneal incision is extended up to the ligament of Treitz, avoiding all vulnerable structures
Again, these first steps are critical. The oncological background of lymphadenectomy needs to be understood. If these first steps cannot be taken due to intestinal obstruction or extreme obesity, an alternative (if necessary) laparotomy must be discussed with the patient. For this reason, the feasibility of laparoscopic surgery must be determined at the beginning of the procedure, just as the possibility of vaginal hysterectomy needs to be determined.
Essentially, preparation is the opening of the peritoneal cover required for surgery. Laparoscopic paraaortic dissection follows a two-tiered approach: first the tent is formed upwards, and then the aortic lymphadenectomy is initiated upwards.
The tent needs to extend to the right side of the patient where the ureter needs to be separated from the right ovarian vein
The difficulty on the right side is always the same: what is the ureter and what is the vein? They look strikingly similar and waiting for the ureters to form is very time consuming. Still, we have to be sure. Sometimes this problem can be resolved simply by widening the dissection at the lateral border of the vena cava.
The right ureter needs to be kept at a distance to expose the psoas space directly to the right side of the inferior vena cava.
This space is easy to open, and - again - the psoas space (this one is more cranial than the first one described in pelvic lymphadenectomy) provides security.
When delineating the right border of the vena cava, care must be taken to identify the branches of the ovarian vein - coagulation of the ovarian vein is required if necessary. Uncoagulated veins increase the risk of tearing, and sometimes emerge directly from the vena cava, creating a hole that cannot be closed by pressure alone.
Likewise, the crossing of the right ovarian arterioles needs to be confirmed and either respected or carefully coagulated and severed.
Ovarian arteries are small, but bleeding is profuse. Sometimes they don't even notice clotting, but lack of clotting is always obvious transection. Their identities are not always possible, but they are always there.
After fixing the "right side" of the tent, the left side needs to be determined.
On the right side, especially the right ureter is easier to see than the left ureter.
First, the branches of the internal mesenteric artery need to be located. In a fairly constant position midway between the aortic bifurcation and the crossing of the left renal vein and extending slightly to the left of the aorta, locate the branch of the inferior mesenteric artery, which is the central reference point for the entire dissection and is key for all subsequent localization . With more experience, one realizes that it is relatively constant. Sometimes it can be seen on a lateral trajectory, but eventually, branches that break away directly from the aorta need to be dissected with blunt instruments. We prefer to start with the medial line of aortic preparation.
Finding the junction of the left renal vein was a challenge. The dissection must not be sharp: cutting to the inferior border of the left renal vein is a disaster that must not happen.
The left renal vein is located 4-5 cm cephalad to the inferior mesenteric artery. Blunt dissection is necessary, however, may cause bleeding from small vessels that may require coagulation, blurring the field of vision and making further dissection more difficult. Achim Schneider's group showed that the learning curve for para-aortic laparoscopic lymphadenectomy takes several years, which is one of the reasons it takes time to get used to in this area.
About 2 cm to the left of the aorta, the left ovarian vein begins to descend from the left renal vein. This corner is the most difficult part of the para-aortic lymphadenectomy.
These lymph nodes are especially important due to the body's lymphatic drainage. If negative, para-aortic lymphadenectomy does analyze complete lymphatic drainage of the uterus.
How best to open the tent is a matter of debate. We have had good experience with first helpers opening tents with two blunt objects as needed. Some surgeons advocate suturing the peritoneal margins to the abdominal wall, while others introduce the retractor through an additional trocar in the upper left quadrant.
Lymphadenectomy can be done from cranial to caudal or from caudal to cranial
Ultimately, the sequence depends on the surgeon's preference and the actual anatomy. Again: Any surgical steps can be described with precision, but not necessarily in sequence.
Aortic dissection is not a problem, and the vena cava needs to be dissected slowly and carefully. Even pulling on the lymphatic tissue can cause the perforator to tear the hole in the vein and possible hemorrhage in the cavity.
The aorta is like a well paved street, easy to navigate. Blunt dissection is possible. The vena cava is more susceptible to injury and blunt dissection should be avoided.
Cavity bleeding requires immediate closure with pressure. About 90% of wounds can be stopped by applying sufficient pressure for at least 5 minutes. Portions that still bleed after prolonged compression need to be closed with 4-0 or 5-0 monofilament sutures.
For small cavity bleeding, pressure is the most effective hemostatic measure. Be careful when using clips and sutures too early. Sometimes they just make things worse.
En bloc lymphadenectomy in the inferior vena cava and paraaortic space is challenging. We recommend a step-by-step approach, taking place in different spaces, and lymph nodes should be removed as they can through a 10 mm trocar at the umbilical level.
This is simultaneously the most challenging and important area of anatomy. Even experienced surgeons still find this field very challenging.
The para-aortic region is below the inferior mesenteric artery (be careful, the ureter is very close to the left edge of the preparation and can be easily injured).
This area - rich in lymph nodes - should be evaluated. Identification of the left ureter is critical.
Paracavity, upper half - note the crossing of the right ovarian artery, branch of the right ovarian vein.
The region of the accessory vena cava to the right of the vena cava-psoas space. Be careful not to damage the right ureter
For this step, excellent visualization, aided by the use of 30° scope and 4K UHD endoscopic camera system is very important. The greatest danger is: bleeding from the perforation of the inferior vena cava, left renal vein, ovarian vein and (if inadvertently exposed) lumbar veins if inadvertently exposed.
The most common source of severe bleeding is a small hole in the lower side of the inferior vena cava because of excessive pulling on the lymphatic tissue, tearing the small perforating vein. Ninety percent of bleeding -- easily diagnosed as a venous bleeding because of its dark blue color -- can be stopped by applying direct pressure to the bleeding site for at least five minutes. Patience is key.
Precautions
1. Identification of pelvic lymph nodes. Most of the pelvic lymphatic system is parallel to blood vessels. Lymph nodes are in the fat tissue around arteries and veins. Lymph nodes in fat tissue are yellowish white or milky white, soft, smooth, and easy to dissociate. 2. Identification of pelvic arteries and veins: there are more lymph nodes than arteries and veins. Familiarity with the distribution of pelvic blood vessels is crucial for lymph node dissection. 3. Two bifurcations and two lacunas: the branches of the great vessels of the pelvis, one is the abdominal aorta divides into the left and right common iliac arteries in the presacral area. The other bifurcation is the bifurcation of the common iliac vessels. The bifurcation of the internal and external vessels is downward and inward, which is the obturator fossa.
- Recommended news
- 【General Surgery Laparoscopy】Cholecystectomy
- Surgery Steps of Hysteroscopy for Intrauterine Adhesion
- [Otolaryngology Nasal Endoscopy] How to Treat Recurrent Rhinitis
- [ENT Surgery: Nasal Endoscopy] Endoscopic Treatment of Nasal Polyps
- [Otolaryngology Nasal Endoscopy] Methods and Precautions for Nasal Bleeding Control under Nasal Endoscopy