【Laparoscopy in Hepatobiliary Surgery】Hypersplenism
Release time: 20 Apr 2023 Author:Shrek
Hypersplenism, referred to as hypersplenism, is a group of syndromes. Many diseases can cause hypersplenism, among which liver cirrhosis caused by various reasons is the most common, such as post-hepatitis cirrhosis, schistosomiasis liver disease, etc. Cirrhosis, portal cirrhosis, etc.; followed by chronic infection, such as malaria; and hereditary spherocytosis in the blood system, autoimmune anemia, idiopathic thrombocytopenic purpura and other diseases can also cause Hypersplenism.
Hypersplenism increases the function of phagocytosis and destruction of blood cells, and more blood cells are retained in the splenic sinus, resulting in decreased peripheral blood cells, increased portal vein pressure, splenic artery blood flow, spleen and portal vein diameter, and hepatic vein wedge pressure. Arterial blood flow is reduced. The clinical manifestations are splenomegaly, one or more blood cells decrease, and bone marrow hematopoietic cells proliferate accordingly.
Currently, splenectomy and partial splenic embolization are the most commonly used clinical treatments for hypersplenism in cirrhosis.
Hypersplenism can be divided into primary and secondary
1. Primary hypersplenism:
Primary hypersplenism refers to hypersplenism of unknown cause. Due to the progress of diagnostics and the development of modern medicine, some hypersplenism that was considered to be primary in the past has now found its cause. Therefore, true primary hypersplenism is less and less common. The diagnosis of primary hypersplenism must exclude all other organic diseases that cause hypersplenism. Therefore, the diagnosis of the disease is a process of exclusion.
2. Secondary hypersplenism
Secondary hypersplenism is hypersplenism caused by a group of disorders. Including infectious diseases such as malaria, typhoid fever and schistosomiasis, tumors such as lymphoma and chronic lymphocytic leukemia, congestion such as portal hypertension caused by various reasons (mainly cirrhosis), etc. In addition, many hematopoietic diseases and immune hemolytic anemia also lead to different degrees of hypersplenism.
Diagnostic criteria
1. If the spleen is enlarged and the spleen is not touched under the ribs, the b-ultrasound examination can be used as a reference.
2. Cytopenia in peripheral blood, in which red blood cells, white blood cells and platelets can be reduced individually or simultaneously.
3. Hyperplastic bone marrow picture.
4. After splenectomy, the peripheral blood can approach or return to normal.
Indications for splenectomy for hypersplenism:
1. Significant splenomegaly, causing obvious compression symptoms.
2. Severe hemolytic anemia.
3. A considerable degree of thrombocytopenia and bleeding symptoms.
4. The neutropenia is extremely reduced, and there is a history of repeated infections.
Hypersplenism Treatment
In terms of treatment, it is also divided into primary and secondary treatment. Secondary hypersplenism is mainly treated for its primary disease. Most of the clinical manifestations of hypersplenism can be alleviated, and splenectomy is rarely required. Once the diagnosis of hypersplenism is established, splenectomy should be performed, the curative effect is obvious, and hormone therapy is often ineffective.
Finally, it must be emphasized that splenomegaly is not necessarily accompanied by hypersplenism, such as splenic cysts, splenic tumors, etc. On the contrary, the reduction of various blood cells that coexists with splenomegaly is not necessarily caused by splenomegaly. The real etiology should be clarified first.
1. Surgical Bypass and TIPS
Shunts mainly include portocaval side-to-side shunt, enterocaval side-to-side shunt and so on. Shunt surgery can reduce the free portal vein pressure and prevent the formation of portal vein thrombosis, but the incidence of postoperative hepatic encephalopathy is high. TIPS has tended to replace surgical shunt in recent years. TIPS can effectively reduce portal vein pressure and reduce the bleeding risk of esophageal and gastric varices, but its therapeutic effect on hypersplenism remains to be clarified. Stent thrombosis and hepatic encephalopathy are the most common complications of TIPS.
2. Splenectomy
Open splenectomy has become the standard treatment for hypersplenism. More recently, laparoscopic splenectomy has been used in patients with splenomegaly and hypersplenism. In a controlled study, half of the patients underwent open surgery and half underwent laparoscopic surgery. Operating times were similar, but blood loss was significantly greater in patients with open splenectomy, laparoscopic surgery resulted in a shorter hospital stay, and anesthesia was simpler. The preoperative average platelet count and white blood cell count were 40 000/μl and 3000/μl, respectively, and both groups rose to the normal range after splenectomy. The main problem with splenectomy is splenic portal vein thrombosis (PVT). In a study of 25 patients with cirrhosis who underwent laparoscopic splenectomy, PVT occurred in 9 patients (36%). The highest risk of PVT occurs within one week after surgery, and the incidence of PVT can be reduced to 4% by anticoagulant therapy.
3. Partial splenic embolism
The principle of partial splenic artery embolization is similar to that of thermal ablation, which can cause local spleen necrosis and reduce the blood flow back to the spleen. This procedure is usually performed interventionally, with a catheter placed in the splenic artery, followed by repeated injections of embolic particles until blood flow to the spleen is reduced by approximately 50%. The degree of splenic infarction reaches 50% to 70% of the spleen volume. Platelets and WBCs are proportional to the volume of the splenic plug. When the embolism volume is >50%, platelet and WBCs counts can return to normal levels. When the embolism volume was ≤50%, there was little change in platelets and WBCs. After prolonged follow-up, counts tended to fall back to the initial range. 80% of patients developed fever and abdominal pain postoperatively, and hospitalization for 2 weeks was not uncommon.
A randomized trial comparing splenic embolization (PSE) with open splenectomy showed a greater increase in platelets and white blood cells with splenectomy. The incidence of PVT was 5% in the embolization group and 15% in the splenectomy group, with no difference in mortality. A nonrandomized trial comparing total splenic artery embolization with partial embolization reported 61 patients, of whom 27 underwent total splenic artery embolization and 34 underwent partial embolization. Results showed that patients who underwent partial embolization experienced more complications, and platelet counts and WBCs were similar between the two regimens. The authors concluded that common splenic arterial embolization is the preferred approach.
About the principle of splenectomy
1. Can prevent fatal upper gastrointestinal rebleeding
In patients with portal hypertension, due to portal hypertension, portal venous blood flow to the cardia is refluxed, and the blood vessels around the cardia are gradually varicose due to long-term high pressure, which is the main cause of bleeding. The blood vessels around the cardia were disconnected, and the factors of reflux were removed. Prevent fatal hemorrhage.
2. Remove the thrombocytopenia caused by hypersplenism and increase the anticoagulant ability of the body.
The spleen is a scavenger that removes old blood cells including platelets. Splenomegaly and hypersplenism can cause excessive platelet clearance. Platelets are the key substance for hemostasis.
3. Correct anemia
Anemia occurs due to excessive clearance of red blood cells by hypersplenism, which exceeds the production capacity of red blood cells. Anemia can cause a series of physical hazards.
4. Can improve liver function and correct blood coagulation
Unlike shunt surgery, devascularization reduces blood flow to the liver, resulting in reduced nutrition and oxygen supply to the liver. Instead, it increases blood flow to the liver and slows down the fibrosis process in the liver.
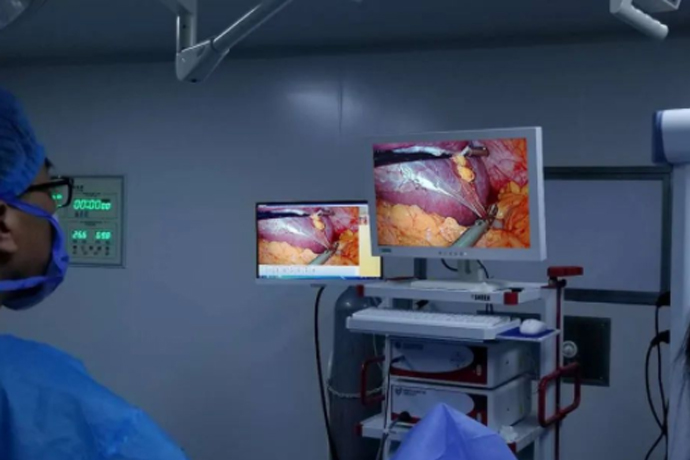
Surgical steps
At present, laparoscopic splenectomy can be divided into anterior approach, posterior approach and combined anterior and posterior approach according to the approach. We routinely take the anterior approach.
1. Incision selection
2. Dissection of the splenocolic ligament
3. Spleen-renal ligament separation
4. Spleen-renal ligament separation
5. Spleen pedicle cut and closed
6. Pericardia vascular detachment
7. Spleen removal
After surgery
1. After the operation, you can usually go back to the general ward or observe in the surgical intensive care unit for one day.
2. Splenectomy greatly stimulates the internal organs of the abdominal cavity (especially the stomach). The gastric tube is inserted into the stomach through the nostrils. There is not much drainage fluid, and it can be removed after the intestinal function is restored (exhaust).
3. The urinary catheter is placed in the bladder for drainage of urine and is usually removed on the 2nd to 3rd day after surgery.
4. 1-2 abdominal drainage tubes will be left in the abdomen to facilitate the outflow of intraperitoneal fluid. Please record the drainage volume and color every day. Normally, it is a small amount of light red or light yellow liquid. We usually recommend removing it after the diet is resumed.
5. It is recommended that you go to the ground early, and it is generally recommended to start on the 2nd to 3rd day after the operation, which can improve blood circulation, prevent thrombosis, and promote the recovery of gastrointestinal function.
6. Patients will be asked to actively perform coughing and deep breathing exercises, and at the same time use nebulized inhalation devices to prevent atelectasis and lung infection.
7. The wound is usually changed on the third day after the operation. If there is abnormal bleeding or exudation, please inform the medical staff.
8. In the early postoperative period, intravenous fluid supplementation, parenteral nutrition solution, acid-suppressing drugs, antibiotics and other treatments are required.
9. Usually after removing the gastric tube, you can start to eat orally. At first, you can start drinking water, and then gradually change to liquid food, semi-liquid food, and finally to a normal diet.
10. If you have no obvious appetite at the beginning, you can take enteral nutrition solution under the doctor's advice.
11. If there is obvious abdominal distension and nausea and vomiting, it is necessary to postpone eating. A small number of patients will have obvious gastrointestinal dysfunction and cannot eat in a short time, and may even re-indwell the gastric tube.
12. A small number of patients have mild fever (body temperature between 37-38 degrees Celsius), which usually relieves within 3-5 days.
13. Most patients will experience weight loss before operation and during the recovery period of operation. This situation will not be relieved for a period of time, but they should try to gain weight after discharge.
Contact your doctor or nurse immediately if:
1. The incision is red and swollen or there is fluid leakage.
2. When the color of the drainage tube liquid changes or the drainage volume increases greatly.
3. Abdominal pain aggravated or new pain symptoms appeared.
4. Nausea, vomiting, diarrhea.
5. Persistent constipation for more than 2-3 days.
6. Other new or unexplained symptoms.
Discharged
When you return to normal diet, normal intestinal function, no complications, and no obvious discomfort, you can consider leaving the hospital. Before discharge, the doctor will give you discharge advice and prescribe the medicines you need to take after discharge. The nurse will check the medicines and discharge time with you. Usually about 2 weeks after surgery.
Special considerations
1. The most common discomfort symptoms after surgery are loss of appetite, abdominal distension, and feeling full. This situation will continue to improve over time. Please eat less and more meals. Don’t worry about slow weight recovery. The most important thing is to ensure daily nutrition Balanced, enough calories to prevent further weight loss.
2. Quit smoking, alcohol, coffee, strong tea, carbonated drinks, hot and sour and other irritating foods, chew slowly, eat light and easy-to-digest foods, avoid full and hard foods, and limit fat intake. Especially don’t eat too much animal fat at one time, avoid too cold food, meet protein supply, often eat lean meat, eggs, chicken, fish, dairy products, soy products, etc., iron-containing foods to meet the needs of hematopoiesis, such as animal liver, blood, Lean meat, eggs, green vegetables, etc. Do not exercise too much after meals.
3. Another common symptom of discomfort is easy fatigue 6-8 weeks after surgery, partly due to surgical reasons, partly due to preoperative weight loss, which will improve over time, and gradually increase the intensity of activity to help improve fatigue.
4. While recuperating at home, you will still feel wound pain. If necessary, you can take painkillers, but one of the side effects of painkillers is constipation. Drink more water and eat crude fiber food to prevent it.
5. Physical exercise can help restore physical strength and improve symptoms. Walking is the best way. Please consult a doctor before doing other more strenuous exercise. Do not overdo it when exercising. Live a regular life and ensure adequate rest and sleep.

- Recommended news
- 【General Surgery Laparoscopy】Cholecystectomy
- Surgery Steps of Hysteroscopy for Intrauterine Adhesion
- [Otolaryngology Otoscopic Section] Excision of Cholesteatoma in the External Auditory Canal
- [Otolaryngology Nasal Endoscopy] How to Treat Recurrent Rhinitis
- [ENT Surgery: Nasal Endoscopy] Endoscopic Treatment of Nasal Polyps