【Laparoscopy in Hepatobiliary Surgery】Enterobiliary drainage
Release time: 04 Apr 2023 Author:Shrek
Biliary enteral drainage is a common operation for the treatment of biliary tract diseases and gastrointestinal diseases. In more than 100 years of clinical application, biliary enteral drainage has been continuously improved. The in-depth study of the structure and its function also has a deeper understanding of the choice of surgical methods and their pros and cons.
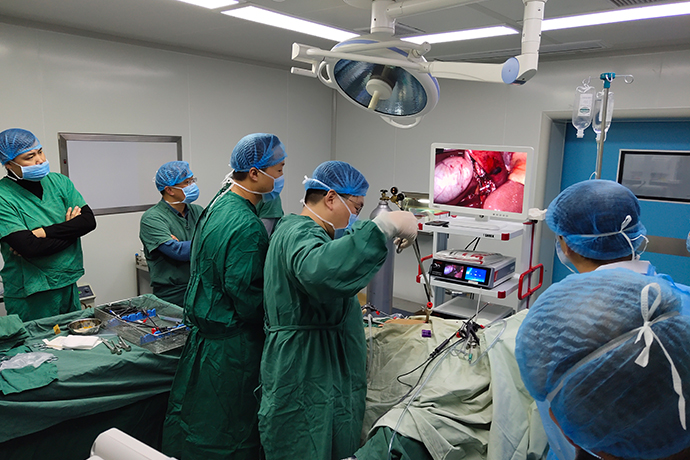
In the operation of intrahepatic bile duct stones, on the basis of removing stones, relieving obstruction, and resecting the lesion, sometimes cholangiojejunostomy, that is, biliary intestinal drainage operation, is required to establish a smooth bile drainage channel. The functions of this operation are as follows:
1.Prevention of restenosis after hepatic and bile duct stenosis incision or plastic surgery (because after incision and plastic surgery of the stenotic bile duct, suturing in situ will inevitably lead to postoperative re-stenosis).
2.Wide anastomotic stoma allows smooth bile drainage and avoids cholestasis, bacterial infection and stone regeneration.
3.The large biliary-enteric anastomosis is conducive to the discharge of small residual stones in the liver into the intestinal tract. In recent years, with the continuous deepening of research on the physiology and pathology of the biliary tract, the indications for various biliary enteric drainage procedures have become clearer, and there have been many innovations in surgical methods.
At present, the common biliary-enteric drainage operations for hepatolithiasis and stricture include: cholangiojejunostomy; intervening jejunal cholangioduodenostomy; intervening jejunal cholangiojejunostomy. Biliary enteric drainage is one of the methods to treat intrahepatic bile duct stones and strictures. If used properly, the postoperative effect is obvious, but if used improperly, the symptoms will be aggravated.
Therefore, it must be emphasized that before the stones are removed and the stenosis is not corrected, it is inappropriate to perform any kind of internal drainage.
Cutting of bile duct
Usually cut at the level of the common hepatic duct. Generally, the upstream of the cystic duct or the right hepatic artery are used as intraoperative markers. From the perspective of bile duct blood supply and surgical operation, it is not meaningful to close the bile duct stump to the pancreas. Cut off the bile duct sharply in one breath. At this time, we must pay attention to whether there is arterial bleeding and bile properties in the bile duct stump (more than 3 o'clock and 9 o'clock). Additional resection is required when there is no arterial bleeding. Flush the bile duct if there is purulent bile. Afterwards, minimal hemostasis is performed with electrocoagulation or sutures. Even if the surgical field of view is deep, 5 mm dorsal dissection of the bile duct is sufficient, and further dissection may affect the blood supply of the bile duct. Use forceps that do not affect the field of view (pug forceps, etc.) to clamp the broken end to prevent bile from contaminating the field of view. Intermittent to be opened to prevent postoperative liver dysfunction.
Jejunum preparation
Lift the stump of the jejunum up from the rear of the colon, being careful not to put tension on it. Sometimes there is tightness of the small mesentery that interferes with venous return to the ascending jejunum. In this case, it is worth noting that as time goes by, the ascending jejunum will become edema and then difficult to anastomose. This is especially likely to occur when the first jejunal artery and vein are preserved (that is, the origin of the mesentery of the jejunum is preserved) and the sacrificed jejunum is too short. During the anastomotic operation, the caliber of the jejunum is often enlarged, so the opening of the jejunum should be smaller than the caliber of the bile duct. Although it can be cut in a straight line, the mucosa is turned outward, and it is troublesome to anastomose. The author prefers to use a full-thickness oval resection of the jejunal wall. In addition, the anterior wall of the jejunum can be fixed with a few full-thickness sutures using 6-0 PDS suture, which is also very effective.
Incision of intestinal wall
The serosa layer of the jejunum is incised in a straight line, and its caliber should be smaller than that of the bile duct. Lift up the mucosa and excise a little to make it the same size as the opening, so as to prevent the mucosa from turning over and affecting the field of vision during the operation.
Posterior wall anastomosis of bile duct and jejunum
Use 5-0PDSⅡ for the suture, and a C-1 (13mm) double-ended needle for the needle. The margins of the suture are roughly 2mm on the bile duct side and 3mm on the jejunum side; the needle distance is about 2mm. Pay attention to the uniform insertion of the needle, and ensure that the full thickness of the bile duct and the full thickness of the jejunum are sutured. In order to expand the space for anastomosis, the hilum of the liver can be blocked with an S retractor, and fixed on the suspension retractor with a curved blood vessel clamp. This frees up the second assistant for timely suction, use of tweezers to help reveal the view, etc. The first assistant uses tweezers to expose the field of vision to facilitate the operator to move the needle, and at the same time cooperates with the thread lifting. Start on the left side of the bile duct (deep to the surgeon). One end of the surgical thread is clamped with forceps as a support thread, and then the needle is delivered from the bile duct to the side of the jejunum (outside-inside-outside-out). After this stitch is finished, the needle is inserted from the outside to the inside just next to it (sewing the back wall of the bile duct). The original circular bile duct was stretched and deformed, and about 3 stitches were carefully sewed from the left side while maintaining this state. This is the most difficult place to suture. At this time, the bile duct and jejunum are separated, and the jejunum side is moved from the inside to the outside, and the bile duct side is moved from the outside to the inside.After about 3 stitches, the jejunum and bile duct are brought close to each other while pulling the suture to make it tense. If the tension is not enough, it will relax, and it will be very difficult to remedy it later. Then, according to the usual method, the needle is delivered from the inside and outside of the jejunum to the bile duct. Start from the left side (deep part) and move the needle evenly to the right side (in front of the eyes), while closely observing the caliber difference between the bile duct and the jejunum, and fine-tuning the distance, so that the caliber difference will disappear when suturing to the right wall. It is difficult to move the needle when reaching the right edge of the bile duct. Move the needle in the order of the outside of the bile duct-inside to the inside-outside of the jejunum, and sew across the right edge under direct vision (observing the lumen). At this time, the suture is pulled out from the outside of the jejunum and then tightened again, clamped with forceps, and pulled back by its weight.
A. In this method, the left side (deep part) is the most difficult to sew. Here, the needle is reliably moved according to the parachute suture method commonly used in the field of vascular surgery.
B. Make the bile duct and jejunum close after about 3 stitches. It is very important to tighten moderately to avoid incomplete sutures.
C. Use the usual sequence from the jejunum to the bile duct.
Anastomosis of hepatic duct and jejunum
The next step is to suture the needle thread coming out from the left edge of the bile duct. Forehand operation, according to the order from the jejunum to the bile duct, that is, outside the inside - inside and outside the needle, toward the right side of the bile duct. In the last 1~2 needles, it is difficult to observe the cavity, so there is no need to lift the back wall during operation. The suture on the right edge was ligated to complete the anastomosis. The anastomosis is completed using only one thread and one ligation. In order to help uniform needle delivery, a support thread can be hung on the right end to facilitate the entry and exit points of the bile duct and jejunum. This support line can be ligated after the posterior wall is sutured. When suturing, place a gauze directly behind the anastomosis. If there is obvious bile contamination, additional suture must be added on the back wall. When the bile duct is anastomosed before pancreaticojejunostomy, the jejunum can be turned sideways or upwards, and the posterior wall can be observed under direct vision. Catheters are generally not inserted into the bile duct.
Anastomosis
A. When suturing the posterior wall, lead the thread out of the jejunum at last, clamp it with forceps for traction.
B. Use the support line at the left end to guide the needle from the jejunum to the bile duct.
C. When suturing the anterior wall, lead the thread out of the bile duct at last, and ligate the thread on the posterior wall, and the anastomosis ends.

- Recommended news
- 【General Surgery Laparoscopy】Cholecystectomy
- Surgery Steps of Hysteroscopy for Intrauterine Adhesion
- [Otolaryngology Otoscopic Section] Excision of Cholesteatoma in the External Auditory Canal
- [Otolaryngology Nasal Endoscopy] How to Treat Recurrent Rhinitis
- [ENT Surgery: Nasal Endoscopy] Endoscopic Treatment of Nasal Polyps