[Gynecological Hysteroscopy] Intrauterine Foreign Body Removal
Release time: 23 Aug 2022 Author:Shrek
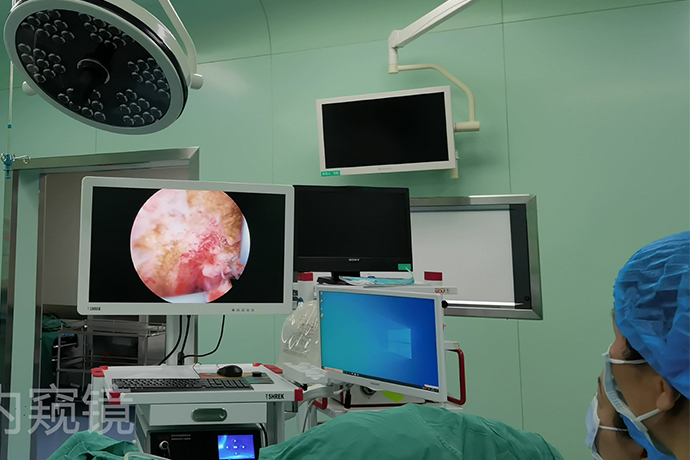
Hysteroscopic intrauterine foreign body removal is a surgical method that uses a hysteroscope and its auxiliary instruments to remove intrauterine foreign bodies under direct vision. Intrauterine foreign bodies include labyrinthine IUDs, residual fetal bone and embryonic residual tissue. The operation under the direct vision of hysteroscope has the advantages of accurate positioning, small trauma, safe operation and high success rate, which is the best choice for removing intrauterine foreign bodies.
Pregnancy residue
Indications
Missed abortion, incomplete abortion, residual placenta, placental adhesions, placenta accreta, etc. are considered to be retained in the uterine cavity by the pregnancy.
Preoperative preparation
1. Inquire about the medical history in detail, check blood β-hCG, and rule out the possibility of trophoblastic tumor.
2. For patients with missed miscarriage or residual embryos for a long time, 3 tablets of Procyone twice a day for 5 to 7 days before surgery to soften the tissue and reduce the adhesion between the tissue and the uterine wall. Except for patients who need to breastfeed after childbirth. For patients with placental residual, placental adhesion or placenta accreta, misoprostol 400 μg orally or rectally can be administered twice a day for 7 days to promote the involution of the uterus and the discharge of residual placental tissue, and at the same time it can dilate the cervix. to facilitate surgical operations.
3. For those with poor postpartum uterine involution and a uterus larger than 10 weeks gestational size, it is advisable to promote uterine involution first and remove most of the placental tissue with forceps under the supervision of B-ultrasound, and then perform hysteroscopy as appropriate after uterine involution.
Surgical steps and techniques
1. Routine disinfection and draping, gynecological examination to understand the position and size of the uterus, exposure and clamping of the cervix, and disinfection of the cervical canal.
2. Use hysteroscopy to examine the cervical canal and uterine cavity to understand the position, size, relationship of the uterine wall and the presence of other combined lesions in the uterine cavity.
3. If the residual pregnancy is small and limited, the pregnancy can be clamped with micro-clamps under the therapeutic hysteroscope.
4. If the residual pregnancy is large, the oval clamp can be used to locate and clamp most of the pregnancy under the supervision of B-ultrasound, supplemented by positioning negative pressure suction. Forceps to remove residual pregnancy.
5. If the residual pregnancy is large and tightly adhered, withdraw the hysteroscope, dilate the cervical canal (usually to size 10, depending on the resectoscope used), and look directly at the bottom of the resectoscope with the ring electrode installed. Under the supervision of B-ultrasound, the pregnancy material is scraped out or excised with an electric cutting ring (for patients with fertility requirements, the pregnancy material should be carefully cut to prevent intrauterine adhesion).
Intraoperative risks and prevention
1. The prevention points of uterine perforation are as follows:
(1) Pay attention to preoperative pretreatment. For patients with long residual pregnancy products, preoperative pretreatment with proganol and misoprostol can greatly reduce the difficulty of surgery and reduce the occurrence of complications. (2) Intraoperative continuous and good ultrasound monitoring. (3) The operator has a full understanding of the position and size of the preoperative ultrasound pregnancy, and combines the findings under hysteroscopy to determine the position and size of the intraoperative pregnancy and the degree of adhesion. (4) A good field of vision under hysteroscopy is helpful for the operator to correctly judge the structure of the pregnancy and the uterine wall. Generally, the pregnancy is yellowish-white or dark red. (5) For those with large and extensive placenta accreta and placental adhesions, those who are difficult to remove at one time, especially breastfeeding patients, do not advocate risky operation under the microscope, and re-operation can be performed in the future to avoid uterine perforation and increase of uterine cavity Possibility of sticking.
2. The prevention points of water poisoning are as follows:
(1) Control the uterine distention pressure, generally 90~120mmHg. Theoretically, the smaller the uterine distention pressure, the smaller the possibility of water intoxication. (2) Physiological saline solution should be used as much as possible. If electric resection is required, plasma electric resection system should be used as much as possible. Using normal saline to distend the uterus will generally not cause hyponatremia. (3) Control the operation time, preferably within 30 minutes, not more than 90 minutes. (4) Record the volume of uterine distended fluid during the operation. When the difference reaches 1500ml, the operation should generally be stopped. (5) Intraoperative dynamic detection of serum potassium and serum sodium levels. (6) Appropriately combine the techniques of oval clamp and negative pressure suction of intrauterine pregnancy under the supervision of B-ultrasound to reduce the time of hysteroscopic operation. (7) For cases with estimated long operation time, furosemide 10-20 mg can be used prophylactically to drain the remaining fluid in the body; it is also possible to use the method of suspending the operation for 10 minutes after the operation for a period of time before continuing the operation. Reduce the risk of water poisoning. (8) During the operation, the water outlet of the hysteroscope should be kept properly open, which can reduce the actual pressure in the uterine cavity as much as possible, maintain a good visual field, and effectively reduce the temperature in the uterine cavity during electric resection.
3. The damage to adjacent organs is mainly due to the failure to detect the perforation of the uterus in time, and the rectum, bowel, bladder and other tissues adjacent to the uterus are electrocuted. The main point of prevention is to detect the perforation of the uterus in time. Uterine perforation with adjacent organ damage should be actively checked (such as laparoscopy, etc.), detected and treated in time to avoid life-threatening complications.
4. Uterine bleeding such as intraoperative operation time is too long, uterine contraction is not good, can lead to more bleeding, intraoperative uterotonic agent and pituitary can be used as appropriate, massage the uterus, stop the operation.
Postoperative treatment
1. For patients who may cause postoperative intrauterine adhesions, intrauterine balloon tubes can be indwelled, sodium hyaluronate can be injected to prevent intrauterine adhesions, and artificial cycles can be given to prevent intrauterine adhesions.
2. For patients with long vaginal bleeding and long operation time, preventive anti-infection should be given as appropriate.
Fetal bone residue
Fetal bone residue after abortion is a rare complication. In the case of artificial abortion, fetal bone residue sometimes occurs, which often causes abnormal uterine bleeding, dyspareunia and secondary infertility.
Indications
Abnormal uterine bleeding, dyspareunia or secondary infertility, suspected fetal bone residual.
Preoperative preparation
1. Sufficient cervical preparation A good cervical preparation is not only conducive to the smooth placement of the hysteroscope, but also for those cases that need to cooperate with the intrauterine forceps to remove the fetal bone, the loose cervical canal makes the oval forceps in the oval forceps. The operation of the uterine cavity is more convenient and safe.
2. Special foreign body removal forceps for hysteroscopy, prepare ring electrode resectoscope.
Surgical steps and techniques
1. Routine disinfection and draping, gynecological examination to understand the position and size of the uterus, exposure and clamping of the cervix, and disinfection of the cervical canal.
2. Use hysteroscopy to examine the cervical canal and the uterine cavity to understand the position, size, relationship with the uterine wall and the presence of other combined lesions in the uterine cavity.
3. Dilation of the cervical canal. When the fetal bone is large or the long axis is perpendicular to the long axis of the uterus, it needs to be expanded to No. 11. After the hysteroscope is positioned, under the supervision of B-ultrasound, use an oval forceps or a hysteroscope. Special foreign body removal forceps can be used to remove the foreign body, or it can be taken out with a hysteroscopic electric resection ring. Those with incarceration need to cut the myometrium, and then clip out or cut by electrocution.

- Recommended news
- 【General Surgery Laparoscopy】Cholecystectomy
- Surgery Steps of Hysteroscopy for Intrauterine Adhesion
- [Otolaryngology Otoscopic Section] Excision of Cholesteatoma in the External Auditory Canal
- [Otolaryngology Nasal Endoscopy] How to Treat Recurrent Rhinitis
- [ENT Surgery: Nasal Endoscopy] Endoscopic Treatment of Nasal Polyps