【Orthopedic Arthroscopy】Arthroscopic anterior and posterior cruciate ligament reconstruction
Release time: 28 Jun 2022 Author:Shrek
What is a cruciate ligament?
The anterior and posterior cruciate ligaments are the most important and strongest ligament structures that maintain the stability of the knee joint. The anterior cruciate ligament (ACL) is tight when the knee is fully extended and relaxed when it is flexed, and its role is to prevent posterior dislocation of the femur, anterior dislocation of the tibia, and excessive extension and rotation of the knee; posterior cruciate ligament The posterior cruciate ligament (PCL) gradually tightens with the flexion of the knee joint, which is beneficial to prevent anterior dislocation of the femur, posterior dislocation of the tibia and excessive flexion of the knee joint.
Anterior cruciate ligament injury is one of the more common knee injuries, and the incidence of combined posterior cruciate ligament injury or pure posterior cruciate ligament injury is also gradually increasing. We used arthroscopic techniques to reconstruct patients with pure anterior cruciate ligament injury, pure posterior cruciate ligament injury, and both anterior and posterior cruciate ligament injuries.
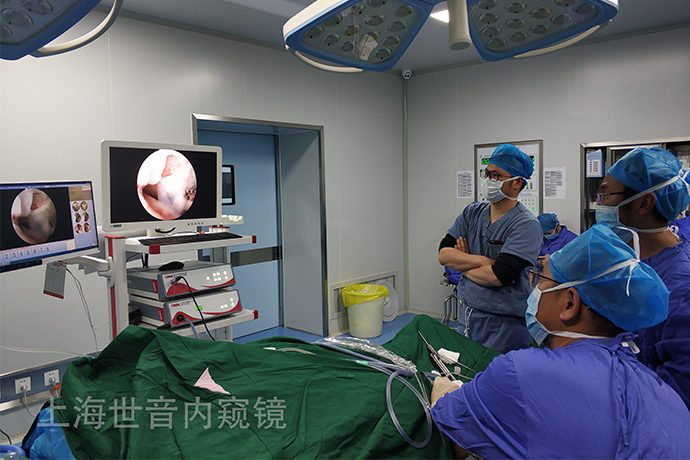
Arthroscopy
First, the PCL fracture was determined by arthroscopic exploration. Single-beam reconstruction is the most commonly used surgery by most scholars. The hamstring tendon was woven into a 4-strand graft, and the PCL stump was preserved as much as possible during exploration.
1. Surgical method
Bone-patellar tendon-bone transplantation: make a longitudinal incision on the lower pole of the patella and the medial side of the tibial tubercle, incise the subcutaneous tissue to expose the patellar ligament, and carefully separate the peritendinous tissue. A 20mm×10mm×8mm bone fragment at the end of the tibial tubercle and the end of the patella were cut with a pendulum saw, and then the middle 1/3 of the patellar ligament was separated from the infrapatellar fat pad. Trim the bone block until it can smoothly pass through the corresponding diameter bone tunnel. Note that two small holes are drilled with a fine Kirschner wire to prepare for traction before correcting the bone fragments at both ends.
Hamstring tendon transplantation: the knee joint is flexed to 90 degrees, and an oblique incision of 5cm length is made on the inner side of the tibial tubercle. The axis is advanced in parallel, and the tendon with a length of about 20-30CM is removed, and the muscle tissue at the end of the tendon is scraped and folded into four strands for reconstruction of PCL and ACL.
ACL Reconstruction: Removal of the remnants of an ACL injury. The intra-articular opening of the tibial tunnel is centered at the center of the ACL stump, near the medial depression of the tibial intercondylar ridge. After determining the location of the intra-articular opening of the tibial tunnel, flex the knee 90° and place the tibial tunnel drill guide from the anteromedial incision. Use a hollow drill with a sleeve to drill the tibial tunnel. Intercondylar femoral plasty is performed on the medial side of the lateral femoral condyle with a bone drill or round chisel. The knee joint is flexed 70°, a guide pin is inserted along the tibial tunnel to the lateral wall of the intercondylar notch, the hollow drill with the mark is pushed along the guide pin to the lateral wall of the intercondylar notch, and the femoral tunnel is drilled with the locator of OFFSET8MM. The knee is flexed 90° to 110°, and a guide wire with a pinhole at the end is inserted through the tibial and femoral tunnels. The silk thread fixed on the patella block of the ligament graft is passed through the eye of the guide needle, and the drill extractor is pulled out together with the guide needle and silk thread, and is passed through the anterolateral thigh. Position the pre-made ligament-osseous junction markings at the entrance of the femoral tunnel. The knee was flexed 90°, and the interface screw was screwed in under direct arthroscopic vision to fix the femoral bone fragment. Distal traction of the graft, check the fixation strength of the femoral interface screw at the tibial end, move 5 to 10 times in the flexion and extension range of the knee parallel joint, so that the movement of the bone fragment in the tibial tunnel does not exceed 2 to 3 mm, and fix the knee at 30 degrees. Tibial end interface screw. Collateral ligament injuries should be repaired or reconstructed separately.
PCL reconstruction: The PCL was cut off at the insertion point of the medial femoral condyle through the anterolateral approach, and the femoral stump and body of the PCL were excised with a planer or radiofrequency. The insertion of the PCL tibial end was removed by radiofrequency through the anterolateral approach. The tip of the tibial tunnel sight was positioned 10mm below the plane of the posterior tibial condyle and 10mm laterally from the posterior median. Connect the elbow positioner (about 50°), and drill the 2.5mm guide wire into the tibial condyle through the cannula. Use an 8mm cannulated drill to drill the tibial tunnel along the guide wire. The femoral tunnel was made, and the center point of the femoral condyle aimer was 12 mm from the posterior border of the cartilage. Connect the elbow locator, cut a 2cm incision above the medial condyle of the femur, drill a 2.5mm guide pin through the cannula, and drill the femoral tunnel along the guide pin with an 8mm hollow drill bit. The grafted ligaments were all fixed with interface extrusion screws, which included cannulated self-tapping metal screws and absorbable cannulated interface screws.
2. Postoperative Rehabilitation
Knee straightening brace was immobilized for 1 day after operation, CPM functional exercise was started on the 3rd day, and extension training and quadriceps functional exercise were started 2 weeks after operation. 6 weeks after the operation, partial weight-bearing was performed, and 10 weeks later, the patients were completely weight-bearing without crutches. If the intraoperative fixation is not satisfactory, the rehabilitation exercise time will be delayed.
3. Results
The evaluation of curative effect was based on knee joint function and modified Lysholm score. Those with scores above 95 were considered excellent, 85 to 94 were considered good, 65 to 84 were considered fair, and less than 65 were considered poor. According to the modified Lysholm score.

- Recommended news
- 【General Surgery Laparoscopy】Cholecystectomy
- Surgery Steps of Hysteroscopy for Intrauterine Adhesion
- [Otolaryngology Otoscopic Section] Excision of Cholesteatoma in the External Auditory Canal
- [Otolaryngology Nasal Endoscopy] How to Treat Recurrent Rhinitis
- [ENT Surgery: Nasal Endoscopy] Endoscopic Treatment of Nasal Polyps