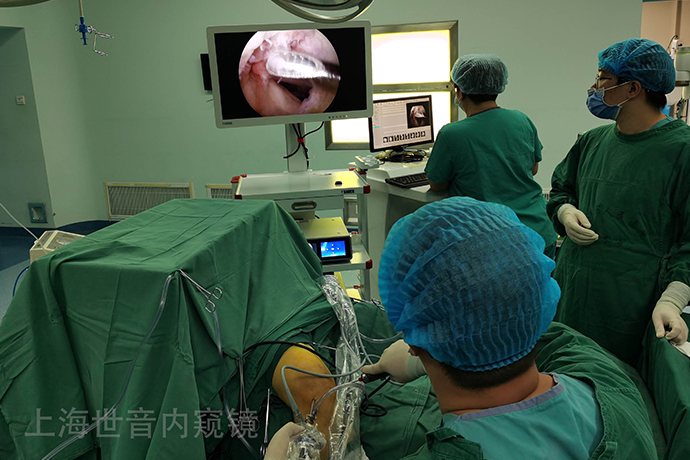
【Orthopedic Arthroscopy】Arthroscopic osteochondral autografting
Release time: 05 Jul 2022 Author:Shrek
Arthroscopic osteochondral autografting is one of the many methods for the treatment of cartilage damage. Osteochondral grafting is the grafting of a healthy plug containing articular cartilage, cartilage tidemarks, and subchondral bone into an area that matches the size of the injury. Advantages of this technique include the use of hyaline cartilage rather than fibrocartilage to repair the defect and maintain joint height and shape. Arthroscopic autografting of osteochondral autografts can be done in one operation at a low cost, and can even be done in outpatient clinics. Panoptical surgery is technically challenging, and due to material limitations, extensive cartilage defects cannot be completely treated with this technique.

Indications and contraindications for surgery
Indications for cartilage autografts include independent, full-thickness cartilage defects ranging from 1 to 2.5 cm in diameter. Large defects (greater than 2.5 cm in diameter) do not respond well. In addition, this technique is generally limited to cartilage lesions with subchondral bone loss no more than 6 mm in depth. Autologous cartilage grafts are also not suitable for knees with damage to adjacent articular cartilage (equivalent to Type IV tibial cartilage damage), multiple Type IV cartilage damage, and unstable or poorly aligned knees. Expected benefits are discounted in patients older than 35 years, and some authors argue that patients older than 50 years should not use this technique. Other contraindications include a history of knee infection, intra-articular fractures, rheumatoid arthritis, and extensive degenerative arthritis. Meniscal tears and ligamentous instability are not absolute contraindications, but such conditions must be addressed during cartilage transplantation. Autologous cartilage grafts are most commonly used on the femoral condyle, although autografts have been reported for tibial plateau, trochlear, and patellar lesions.
Instrument
The osteochondral graft (COR) system can precisely obtain the osteochondral plug column and implant it into the same size hole in the defect area. The distinguishing features of the COR system are the cutting teeth of the extraction sleeve for more precise depth of cut, and a well-designed drill bit for defect area preparation. This drill makes it easier to make the recipient hole perpendicular to the adjacent articular cartilage surface, so that the size of the recipient and the donor site is more matched.
surgical technique
A thorough knee arthroscopy evaluation is performed first. When a localized, full-thickness cartilage defect is found, it is important to explore all areas of the knee joint, including the posterior recess and inferior meniscus, to detect and remove any mobile cartilage debris. Arthroscopic grafting is suitable for most defects; however, large and more posterior defects require extreme flexion of the knee to achieve an angle perpendicular to the articular cartilage and sometimes limited incision of the joint to achieve this angle. Use a lumbar puncture needle to determine the optimal angle of the approach, ensuring that the approach is perpendicular to the recipient and donor sites.
Arthroscopic autologous cartilage transplantation is performed in four steps:
1. Assess and prepare the defect area;
2. Determine the number of grafts;
3. Take material;
4. Prepare the implantation area and implant autologous emboli.
Assessment and preparation of the defect area
The knee joint and defect area should be carefully evaluated to ensure that selection criteria are met and that there are no contraindications to this procedure. Preparation of the defect area consists of removing all free articular cartilage debris and creating a vertical cartilage wall at the edge of the defect with a curette or an arthroscopic knife. The residual articular cartilage on the subchondral bone surface is removed, but extensive bleeding on the bone surface should be avoided. For better planning of bone grafting, the initially implanted post should be placed in the most anterior part of the defect area immediately adjacent to the articular cartilage.
Determining the number of implanted bones
Once the defect boundary is determined, a probe can be used to estimate the number of bone grafts required, or a sampling cannula can be used to measure the size and depth of the defect to determine which shape of the post is most suitable for the defect. The depth of the defect area can be estimated with the COR system, that is, with a probe or a measuring ruler on the side of the sampling cannula. In general, a series of 6 mm diameter graft posts can be arthroscopically implanted and filled in the defect area. Larger pegs are available, but they often require small incisions to implant and tend to involve high-load-bearing cartilage in the donor site.
The depth of the defect area should also be analyzed. Most of the defects had no obvious bony defect. In these cases, the standard 8mm cannula depth was sufficient to fill the defect area. However, some defects (particularly those of chondroitritis dissecans) have significant bony defects and must be managed. In this case, bone grafting in the bone defect area can be performed in one operation, and cartilage grafting can be performed later, or a longer plug can be obtained by using a sampling cannula of different depths, and the graft can be placed in place so that the cartilage surface is in contact with the surrounding cartilage. The surface is flat, but exposes the cancellous bone under the columella cartilage to the base of the bony depression .
In transplantation, it is also important to assess the shape of the donor and recipient articular cartilage to achieve the best possible match of the cartilage surfaces. For large defects, the use of multiple pegs can effectively reconstruct the original shape of the condyle. Although better reconstruction of the shape can be achieved with a smaller plug, the benefits are negated by a reduction in the strength and stability of the graft plug and an increase in surgical steps.
- Recommended news
- 【General Surgery Laparoscopy】Cholecystectomy
- Surgery Steps of Hysteroscopy for Intrauterine Adhesion
- [Otolaryngology Otoscopic Section] Excision of Cholesteatoma in the External Auditory Canal
- [Otolaryngology Nasal Endoscopy] How to Treat Recurrent Rhinitis
- [ENT Surgery: Nasal Endoscopy] Endoscopic Treatment of Nasal Polyps