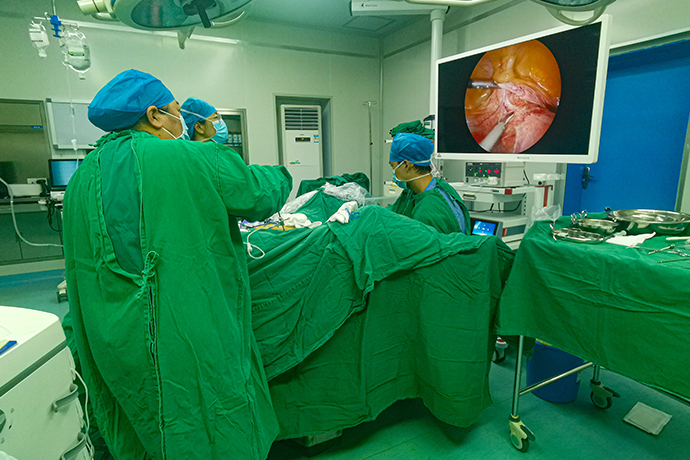
【Gynecological Laparoscopy】Conservative surgery for tubal pregnancy
Release time: 26 Oct 2021 Author:Shrek
Indications
1. There are fertility requirements, especially those whose contralateral fallopian tube has been removed or has obvious disease.
2. Local bleeding in tubal pregnancy is not active, the tube wall is not broken or the breach is small.
3. Exclude intrauterine pregnancy.
Contraindications
1. Rupture of tubal pregnancy leads to a large amount of intra-abdominal bleeding or is accompanied by obvious shock, which is a relative contraindication to laparoscopic surgery.
2. Conservative surgery should not be performed for patients with severe damage to the affected side of the interstitial fallopian tube.
3. Recurrent ectopic pregnancy and tubal tuberculosis.
Surgical steps and techniques
1. Aspirate the blood and blood clots in the pelvic and abdominal cavity, and separate the adhesions around the affected side of the fallopian tube.
2. Grasp the proximal part of the fallopian tube where the gestational sac is implanted with non-invasive forceps, and first use unipolar bipolar electrocoagulation to coagulate the enlarged fallopian tube part to be incised.
3. Use an electric coagulation hook to cut the wall of the fallopian tube longitudinally on the opposite side of the mesangium. If there are relatively large blood vessels on the surface, use monopolar or bipolar coagulation for electrocoagulation.
4. Inject water between the fetal mass and the wall of the fallopian tube to make the fetal mass and the wall of the fallopian tube bulge out on its own after separation. This method has less bleeding.
5. If the incision is less than 5mm, no suture is needed, and if the incision is greater than 5mm, it can be sutured with 1 to 3 stitches.
6. Inject 20 mg of methotrexate (MTX) into the proximal end of the tubal pregnancy lesion under the serous membrane.
7. Flush the abdominal cavity, check for active bleeding, and apply sodium hyaluronate gel on the wound to prevent adhesion.
Intraoperative risks and prevention
1. Wound hemorrhage. Before the pregnancy fetal mass is separated from the fallopian tube wall, if the fetal mass is forcibly torn off from the tube wall, it may cause active bleeding on the wound and not easy to stop bleeding.
Preventive measures: Avoid forced tearing to remove pregnancy tissue, and make full use of the water separation method. Bleeding on free-edge wounds should be stopped by intermittent suture with 3-0 absorbable thread; bleeding on the mesangial side of the wound can be stopped by electrocoagulation or with U-shaped sutures on the mesangial side.
2. Residual villi in the fallopian tube. Villi tissue is easy to remain during conservative surgery for tubal pregnancy, resulting in persistent ectopic pregnancy.
Preventive measures: The embryo implantation site is often located at the proximal end of the fallopian tube, so the embryo extraction incision should be as close as possible to the swelling near the end of the uterus, to completely remove the visible villi, and inject MTX into the proximal end of the pregnancy lesion to kill the remaining villi tissue.
Precautions after operation
After the fallopian tube incision is sutured and local hemostasis, the pelvic and abdominal cavity is fully rinsed with water, and the fetal mass is sent for pathological examination. Pay attention to whether there are residual villi in the sulcus of the colon.
During the operation, it is necessary to fully understand the pelvic condition, thoroughly clean up the pelvic and abdominal lesions and hemorrhage, dredge the fallopian tubes, loosen the adhesion zone, and minimize or avoid the risk of ectopic pregnancy again.
After the operation, the blood β-hCG should be closely observed until it is negative (on the first postoperative day, once a week after discharge until the β-hCG is normal). If β-hCG does not decrease or increase continuously, prompt treatment is required.
Infertile patients underwent hysterosalpingography three months after surgery to observe the shape and patency of the fallopian tubes.

1. There are fertility requirements, especially those whose contralateral fallopian tube has been removed or has obvious disease.
2. Local bleeding in tubal pregnancy is not active, the tube wall is not broken or the breach is small.
3. Exclude intrauterine pregnancy.
Contraindications
1. Rupture of tubal pregnancy leads to a large amount of intra-abdominal bleeding or is accompanied by obvious shock, which is a relative contraindication to laparoscopic surgery.
2. Conservative surgery should not be performed for patients with severe damage to the affected side of the interstitial fallopian tube.
3. Recurrent ectopic pregnancy and tubal tuberculosis.
Surgical steps and techniques
1. Aspirate the blood and blood clots in the pelvic and abdominal cavity, and separate the adhesions around the affected side of the fallopian tube.
2. Grasp the proximal part of the fallopian tube where the gestational sac is implanted with non-invasive forceps, and first use unipolar bipolar electrocoagulation to coagulate the enlarged fallopian tube part to be incised.
3. Use an electric coagulation hook to cut the wall of the fallopian tube longitudinally on the opposite side of the mesangium. If there are relatively large blood vessels on the surface, use monopolar or bipolar coagulation for electrocoagulation.
4. Inject water between the fetal mass and the wall of the fallopian tube to make the fetal mass and the wall of the fallopian tube bulge out on its own after separation. This method has less bleeding.
5. If the incision is less than 5mm, no suture is needed, and if the incision is greater than 5mm, it can be sutured with 1 to 3 stitches.
6. Inject 20 mg of methotrexate (MTX) into the proximal end of the tubal pregnancy lesion under the serous membrane.
7. Flush the abdominal cavity, check for active bleeding, and apply sodium hyaluronate gel on the wound to prevent adhesion.
Intraoperative risks and prevention
1. Wound hemorrhage. Before the pregnancy fetal mass is separated from the fallopian tube wall, if the fetal mass is forcibly torn off from the tube wall, it may cause active bleeding on the wound and not easy to stop bleeding.
Preventive measures: Avoid forced tearing to remove pregnancy tissue, and make full use of the water separation method. Bleeding on free-edge wounds should be stopped by intermittent suture with 3-0 absorbable thread; bleeding on the mesangial side of the wound can be stopped by electrocoagulation or with U-shaped sutures on the mesangial side.
2. Residual villi in the fallopian tube. Villi tissue is easy to remain during conservative surgery for tubal pregnancy, resulting in persistent ectopic pregnancy.
Preventive measures: The embryo implantation site is often located at the proximal end of the fallopian tube, so the embryo extraction incision should be as close as possible to the swelling near the end of the uterus, to completely remove the visible villi, and inject MTX into the proximal end of the pregnancy lesion to kill the remaining villi tissue.
Precautions after operation
After the fallopian tube incision is sutured and local hemostasis, the pelvic and abdominal cavity is fully rinsed with water, and the fetal mass is sent for pathological examination. Pay attention to whether there are residual villi in the sulcus of the colon.
During the operation, it is necessary to fully understand the pelvic condition, thoroughly clean up the pelvic and abdominal lesions and hemorrhage, dredge the fallopian tubes, loosen the adhesion zone, and minimize or avoid the risk of ectopic pregnancy again.
After the operation, the blood β-hCG should be closely observed until it is negative (on the first postoperative day, once a week after discharge until the β-hCG is normal). If β-hCG does not decrease or increase continuously, prompt treatment is required.
Infertile patients underwent hysterosalpingography three months after surgery to observe the shape and patency of the fallopian tubes.

- Recommended news
- 【General Surgery Laparoscopy】Cholecystectomy
- Surgery Steps of Hysteroscopy for Intrauterine Adhesion
- [Laryngoscopy in Otolaryngology] Tonsillectomy
- [Otolaryngology Otoscopic Section] Excision of Cholesteatoma in the External Auditory Canal
- [Otolaryngology Nasal Endoscopy] How to Treat Recurrent Rhinitis