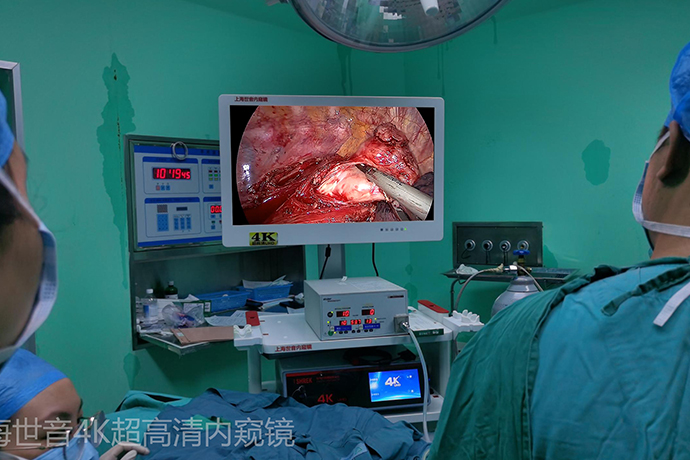
[General Surgery Laparoscopy] 4K ultra-high definition laparoscopic abdominal wall hernia mesh repair
Release time: 03 Apr 2024 Author:Shrek
Inguinal hernia
Inguinal hernia refers to a mass formed by the internal organs in the abdominal cavity protruding to the body surface through a defect in the groin area. It is commonly known as "hernia" and is called "Young Pioneers" in southern Fujian dialect. The groin area is the triangular area located at the junction of the lower abdominal wall and thighs. Common in children and the elderly, there are two types of inguinal hernia: congenital and acquired. The incidence ratio between men and women is 15:1.
Why does a "hernia" occur?
It is mainly related to weak abdominal wall and increased intra-abdominal pressure.
Congenital factors, such as patent processus vaginalis, inguinal dysplasia, etc.;
Acquired factors, such as advanced age, poor growth and development, poor nutrition and metabolism, and other certain diseases;
Other predisposing factors: such as long-term smoking, obesity, constipation, pregnancy, abdominal tumors, ascites, etc.
What are the main surgical methods for hernia?
Hernia surgery methods are divided into: open surgery and laparoscopic (minimally invasive) surgery.
The main open surgeries include Ligenstein hernia repair and open preperitoneal repair.
Laparoscopic (minimally invasive) surgeries include: laparoscopic transabdominal preperitoneal patch repair (TAPP), total extraperitoneal patch repair (TEP), and pediatric laparoscopic hernia repair.
What are the advantages of laparoscopic hernia repair?
Traditional surgical hernia surgery or laparoscopic hernia surgery are both equally effective. Surgery can be completed using local anesthesia, spinal anesthesia or epidural anesthesia, and the cost is relatively low. Laparoscopic surgery is usually performed under general anesthesia and is relatively expensive; however, laparoscopic surgery patients are usually more comfortable during the operation, and the incisions are smaller and more beautiful. Bilateral inguinal hernias and occult hernias can be treated through the same incision without causing damage. The natural structure of the groin area does not affect the cremasteric reflex and can reduce the impact on male reproductive function. Postoperative pain is mild and recovery is quick. Most people can go out and move around on the day or the next day after surgery, and hospitalization is enough for 1-2 days. Hospital discharge, low complications and low postoperative recurrence rate.
What is the difference between TAPP and TEP in laparoscopic hernia repair?
Laparoscopic inguinal hernia repair
Laparoscopic inguinal hernia repair is a safe, technically sound and tension-free repair surgery. Mainly includes two methods:
1. Transabdominal preperitoneal patch implantation (TAPP), because it enters the abdominal cavity, is easier to detect bilateral hernias, compound hernias and occult hernias. It is also easier to observe and handle cases of incarcerated hernias and cases where hernia contents are difficult to return.
2. Total extraperitoneal patch implantation (TEP) does not enter the abdominal cavity and has minimal interference with intra-abdominal organs.
The TEP surgical operation is basically the same as the TAPP surgical operation. There is no significant difference between the two surgical methods in terms of postoperative complications, hospitalization time, and recurrence rate. Because TEP surgery does not enter the patient's abdominal cavity, it reduces interference with the abdominal cavity, avoids damage to abdominal organs and postoperative abdominal adhesions, and avoids peritoneal sutures. The operation time is relatively shorter and the trauma to the patient is less. TAPP surgery requires entering the abdominal cavity. Usually the anatomy is clear and the landmark structure is clear, so it is more suitable for hospitals that have just launched laparoscopic hernia repair.
When TEP surgery was carried out in the early days, it was difficult to learn because the anatomical planes were unclear. After mastering this technique, more doctors will choose this surgical method.
Advantages of 4K Ultra HD Laparoscopic Inguinal Hernia Repair
(1) The incision is small, the pain is light, and it is beautiful.
(2) Avoid tissue damage, nerve damage, and incision infection caused by incisions.
(3) The local tension and foreign body sensation are slight.
(4) The space is large, the field of view is super clear, the anatomical landmarks are obvious, and the patch is easy to place and flatten.
(5) Whether there is an occult hernia can be detected during the operation and treated promptly.
(6) There are advantages in treating bilateral hernias, compound hernias and recurrent hernias.
(7) Patients can resume non-restrictive activities earlier after surgery.
Surgical procedure
Identify ligaments
①Mid-umbilical ligament: Located in the midline, it is the residual trace after urachal occlusion.
② Medial umbilical ligament: The peritoneal fold covering the surface of the occluded umbilical artery is located on both sides of the middle umbilical ligament, and the bladder is located between the two medial umbilical ligaments.
③Lateral umbilical ligament: The peritoneal fold covering the surface of the inferior epigastric artery, located outside the medial umbilical ligament. Usually, the peritoneum is incised in an arc 3cm from the upper edge of the hernia defect. The inside should not exceed the medial umbilical ligament to avoid damaging the bladder. When incising the peritoneum in the middle, the inferior epigastric artery should be avoided.
Isolate the preperitoneal space
The separation range of the preperitoneal space is from the symphysis pubis internally, from the psoas major muscle and the anterior superior iliac spine externally, at least 3cm above the symphysis muscle, 3cm below the pubic pectineal ligament medially and inferiorly, and to the "pelvic wall" of the spermatic cord laterally and inferiorly. "6~8cm to ensure that a 10cm x 15cm patch can be implanted.
Tile fixed patch
Usually, a patch of 10cm×15cm is used and trimmed appropriately according to the patient’s condition. Patch that is too small is one of the important reasons for postoperative recurrence. The patch can be fixed using a hernia fixator or sutures. The patch should be fixed with the rectus abdominis, pectineal ligament and syndesmotic muscles, and the coverage and fixation with the pubic tubercle is particularly important, because most recurrences occur in the direct hernia triangle next to the pubic tubercle. For bilateral hernias, the pubovesical space should be fully dissected so that the preperitoneal spaces on both sides are connected, and the inner side of the patch overlaps at the pubic symphysis. When stapling the upper part of the patch, damage to the inferior epigastric artery should be avoided, and when stapling the lower part, the crown of death, danger triangle, and pain triangle areas should be avoided.
Usually the patch is laid flat on the spermatic cord and spread as flat as possible. Curled patches can cause postoperative recurrence. You can also cut a small opening in the patch, wrap it around the spermatic cord, and then fix it. This is equivalent to strengthening the posterior wall of the inguinal canal and simultaneously reshaping the inner ring opening. Since stapling the patch with a stapler may cause postoperative pain, fibrin glue is currently used abroad to bond the patch.
Close the peritoneum
The peritoneum can be closed using staples or sutures. The peritoneum should be fully closed to avoid contact between the patch and the abdominal contents, otherwise it may cause postoperative intestinal obstruction or even intestinal leakage.

- Recommended news
- 【General Surgery Laparoscopy】Cholecystectomy
- Surgery Steps of Hysteroscopy for Intrauterine Adhesion
- [Otolaryngology Nasal Endoscopy] How to Treat Recurrent Rhinitis
- [ENT Surgery: Nasal Endoscopy] Endoscopic Treatment of Nasal Polyps
- [Otolaryngology Nasal Endoscopy] Methods and Precautions for Nasal Bleeding Control under Nasal Endoscopy