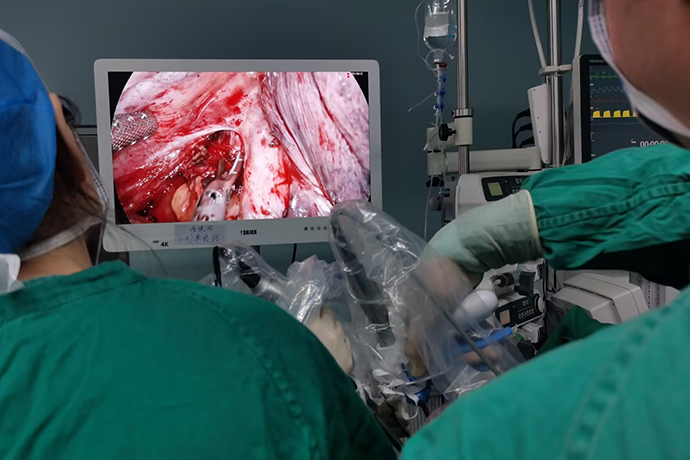
[Thoracic Surgery and Thoracoscopy] 4K ultra-high definition chylothorax surgery
Release time: 27 Feb 2024 Author:Shrek
Chylothorax is caused by rupture or obstruction of the thoracic duct due to different reasons, causing chylofluid to overflow into the chest cavity. The thoracic duct is the largest lymphatic vessel in the body, with a total length of about 30~40cm. It is divided into two parts, one is the manifestation of the primary disease; the other is the symptoms of chylothorax itself. Traumatic thoracic duct rupture causes rapid overflow of chylous fluid, which can produce compression symptoms such as shortness of breath, dyspnea, and mediastinal shift. Disease Description Chylothorax is caused by rupture or obstruction of the thoracic duct due to different reasons, causing chylofluid to overflow into the chest cavity. The thoracic duct is the largest lymphatic vessel in the body, with a total length of about 30~40cm. Although rare, chylothorax is a huge problem in thoracic surgery because it can lead to immunocompromise, pneumonia, and mortality rates as high as 30%.
Definition and classification
The leakage of lymphatic chylofluid that flows back through the thoracic duct and accumulates in the pleural cavity is called chylothorax. Its occurrence is related to injury or occlusion of the thoracic duct. According to the cause, it can be divided into primary chylothorax and traumatic chylothorax.
Traumatic: Postoperative chylothorax is the most common type of traumatic chylothorax. Most of them are accidental injuries during thoracic surgery, especially after esophagectomy, and lung cancer resection accompanied by mediastinal lymph node dissection or en bloc resection. In addition, it can be seen in cardiac, aortic, mediastinal and sympathetic nerve surgeries. Occasionally seen after sclerotherapy injection for recurrent varicose veins, or after translumbar aortography, neck lymph node dissection, or central venous catheterization. 20% of traumatic chylothorax is caused by trauma. When penetrating trauma occurs in the neck, chest or abdomen, the thoracic duct can be directly torn. Blunt trauma, such as severe coughing or thoracic duct traction, can also cause thoracic duct rupture.
Congenital: Bilateral chylothorax caused by congenital lymphangiectasia, which is extremely rare.
Obstructive: When a tumor appears in the thoracic cavity or retroperitoneal space, compressing or infiltrating the thoracic duct, the thoracic duct will be obstructed, resulting in the rupture of its proximal and side branches, allowing chylous fluid to flow into the thoracic cavity. More than 50% are caused by tumors, of which lymphoma accounts for 70%. Other factors include venous thrombosis, pulmonary lymphangioleiomyomatosis, metastatic cancer, lymphadenitis and infections such as tuberculosis and filariasis.
Non-surgical treatment
For symptomatic chylothorax, closed chest drainage should be performed first to relieve intrathoracic hypertension caused by pulmonary compression respiratory distress. Conservative treatment is possible for chylothorax with daily drainage volume less than 500 ml, including:
1. Dietary management: Reduce oral and intestinal fat intake to reduce the production of chylofluid and drug treatment. Commonly used drugs are octreotide and somatostatin, which can inhibit the secretion of growth hormone, glucagon, insulin and lymphatic excretion. .
2. Pleurodesis: It can be used alone or combined with thoracic duct ligation to treat refractory chylothorax. Commonly used pleurodesis drugs include tetracycline, nocycline, bleomycin, OK-432, povidone-iodine, and talc.
Surgical treatment
1. Thoracic duct ligation: 4K ultra-high-definition video-assisted thoracoscopy (VATS) or direct chest duct ligation under direct vision can effectively treat chylothorax. If chylous leakage occurs in multiple locations or the site of chylous leakage cannot be determined, the thoracic duct proximal to the aortic hiatus can be directly ligated.
2. Thoracoabdominal shunt: Mainly used to treat refractory chylothorax, including Denver thoracoabdominal shunt and selective passive LeVeen thoracoabdominal shunt. The placed thoracic duct shunt can drain the chylofluid to where it can be absorbed. Abdominal cavity. There is a large amount of literature proving that this method can effectively treat chylothorax in patients with total parenteral nutrition. However, due to its many complications (including shunt occlusion, fibrin clot, infection, skin erosion, pneumoperitoneum, etc.), it should be used with caution.
3. Thoracic duct percutaneous embolization: It can be used to treat refractory chylothorax where the location of galactorrhea has been confirmed. Although it is technically difficult to use a microcatheter to connect the thoracic duct and use a metal coil for embolization treatment, the success rate of catheterization is 67% and the cure rate is as high as 90%, which makes it a good prospect in the treatment of chylothorax. . Based on previous data from the literature on the treatment of chylothorax, Figure 1 provides “ideal” selection criteria for the treatment of chylothorax.
Common complications of chylothorax include:
Chylofluid, a liquid containing fat and protein, is mostly milky white. When it solidifies and blocks the drainage tube, chylofluid compresses the chest cavity and worsens the original symptoms. After thoracic duct ligation, the duct ruptures, causing chylous fluid to overflow and aggravating the chylous fistula.
Indications for surgical thoracoscopic thoracic duct ligation
Surgical treatment is considered to mean:
Greater than 1000-1500mL. Excrete chyle every day
Output up to 1000ml/day in 5 treatment days
Leakage persists for more than 2 weeks (100 ml/day > 2 weeks)
Clinical deterioration, such as malnutrition or metabolic problems
Surgical treatment of chylothorax
The key point is that fasting and eating anything can increase the amount of lymphatic reflux and increase the outflow of the leak, which will prevent the leak from healing for a long time.
Before surgical treatment, conservative treatment is required for up to 14 days. During this period, 25-50% of leaks can heal on their own, and the rest require surgical treatment. If the daily drainage volume is greater than 500ml and has been for more than 2 weeks, it indicates that surgical treatment is necessary, unless other pathological changes exist.
Surgical method: Inject 100-200ml of olive oil through the gastric tube 2-3 hours before the operation, which can fill the thoracic duct with chyle and make it easier to identify. The remaining olive oil in the stomach should be sucked out before anesthesia. Another method is to inject 1% methylene blue into the leg, which can stain the thoracic duct within 5 minutes and maintain it for 12 minutes. The disadvantage is that other tissues can also be stained. It is recommended to take whole milk or cream orally 30 minutes before the operation, and infuse the chest with saline during the operation to help detect chyle leaking from the thoracic duct.
No matter which side of chylothorax it is, the right thoracotomy is adopted and the thoracic duct is ligated on the diaphragm. In more than 60% of patients, there is only one thoracic duct between the 12th and 8th thoracic vertebrae, which is the thoracic duct in 40% of patients. The caudal end is a branching structure, so it is important to perform bulk ligation to avoid missing larger branches. The operation uses a small right anterolateral incision to remove the fibrous deposits on the pleura, release the pulmonary ligament, and use non-absorbable sutures to ligate all the tissues between the azygos vein and the aorta. After the ligation is completed, the thoracic duct, azygos vein, and intercostal space The small anastomotic branches between the veins and lumbar veins quickly establish compensatory collateral pathways.
Chylothorax caused by malignant tumors should be treated with radiation to promote the closure of thoracic duct and lymphatic fistulas.
Postoperative care precautions:
After pleural effusion drainage, attention should be paid to whether the patient's drainage tube is unobstructed, the nature of the drained fluid, the replacement of dressings, etc.; the patient should fast within 2 weeks after catheter ligation, and use a gastric tube to aspirate the gas and gas in the gastrointestinal tract. fluids, adequate and effective gastrointestinal decompression, and complete parenteral nutritional support. If the amount of drainage decreases 2 to 4 weeks after surgery, you can eat according to the doctor's advice.
Diet:
For patients with good gastrointestinal function and the ability to eat, they can eat a low-fat or fat-free diet, mainly high-quality fats such as palm kernel oil and coconut oil, avoid fatty meat, butter, fried foods, etc., and provide intravenous nutrition and supplementation. A variety of amino acids, vitamins, electrolytes and sufficient water.

- Recommended news
- 【General Surgery Laparoscopy】Cholecystectomy
- Surgery Steps of Hysteroscopy for Intrauterine Adhesion
- [Otolaryngology Nasal Endoscopy] How to Treat Recurrent Rhinitis
- [ENT Surgery: Nasal Endoscopy] Endoscopic Treatment of Nasal Polyps
- [Otolaryngology Nasal Endoscopy] Methods and Precautions for Nasal Bleeding Control under Nasal Endoscopy