[Gynecological Hysteroscopy] Hysteroscopic Ring Removal
Release time: 27 Sep 2022 Author:Shrek
Everyone is familiar with the word "birth control ring". Medically, we call it "intrauterine device".
In the 1970s and 1980s, family planning was listed as a basic state policy. Many people use IUDs placed by women for contraception, so that it will not affect future pregnancy, and can easily prevent pregnancy. According to statistics, from 1980 to 2009, Chinese women used IUDs 286 million times. Thirty or forty years have passed, and women in "Sheung Wan" have gradually entered menopause. Due to the neglect of the IUD and the lack of knowledge about the IUD, many women still don't realize that the IUD is not "once and for all", and regular review is required to know whether the IUD has been displaced or fallen off. Otherwise, it will seriously endanger your own health.
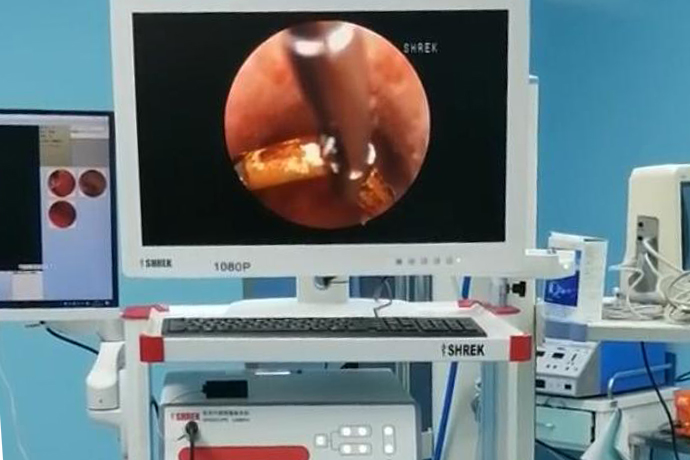
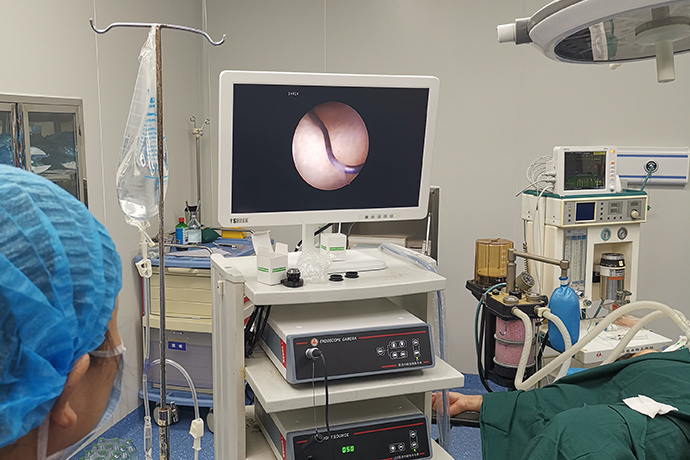
A hysteroscope is a fiber-optic endoscope. Hysteroscopy refers to the application of dilatation media to dilate the uterine cavity, and the optical fiberglass speculum inserted into the uterine cavity through the vagina to directly observe the physiological and pathological changes of the cervical canal, internal cervical orifice, uterine cavity and fallopian tube opening, so as to identify the pathological changes. The tissue is intuitively and accurately obtained and sent for pathological examination. At the same time, it can also be directly operated under the hysteroscope. It has the advantages of clear vision, high lesion identification, less trauma, quick postoperative recovery, and day surgery can be carried out. Popularity is high. Hysteroscopy and surgery have almost become a hurdle that female patients must face.
Use hysteroscopy for difficult intrauterine devices (IUDs). Mostly due to menorrhagia or failure to take the device for family planning more than 2 times. Hysteroscopy found that the IUD was twisted, deformed, and fractured, and some only had residual IUD, some implanted in the myometrium, and some swam out of the uterine cavity. Hysteroscopy can directly observe the shape and position of the IUD in the uterine cavity, and whether it is implanted in the uterine wall, so as to determine the way and method of taking the IUD.
Common side effects or complications after IUD placement are:
1. Abnormal uterine bleeding, pain.
2. IUD incarcerated, IUD ectopic.
3. Ectopic perforation.
4. Pregnancy with a device (referring to the coexistence of pregnancy and an intrauterine device), etc.
Situations in which an IUD should not be placed:
1. Acute pelvic inflammatory disease; acute vaginitis.
2. Severe cervical erosion, menorrhagia or irregular bleeding, uterine fibroids, narrow cervix.
3. Women with serious systemic diseases should not have the ring, otherwise, it will lead to aggravation of inflammation and increased menstrual flow.
In which cases to take the ring:
1. Those who have put the ring for more than 5~10 years and require a new ring.
2. Those who have irregular vaginal bleeding or other symptoms after treatment fails. Vaginal bleeding or accompanied by infection, the ring should be removed in time.
3. Those who wish to have children again.
4. One year after sterilization. For more than half a year of menopause, it is recommended to take a ring.
5. Those who have serious side effects and change contraceptive methods.
6. Those who are pregnant with a ring can be taken out during abortion.
Ectopic IUD refers to:
The IUD leaves the normal position of the uterine cavity and is partially or completely embedded in the muscle layer, or ectopic to the abdominal cavity, broad ligament, bladder, rectum, etc. When the IUD is ectopic, not only can it no longer play a contraceptive role, but it will also bring trouble to the user.
Symptoms of an ectopic IUD:
1. Abdominal pain.
2. Pregnancy with device.
3. Menstruation is dripping.
IUD ectopic causes:
1. The risk of ectopic placement of IUD during lactation increases.
2. The IUD is too large or placed in an improper position.
3. The shape of the IUD is not compatible with the shape of the uterine cavity.
According to the degree of ectopic can be divided into three categories:
(1) Partial incarceration of the IUD: The IUD is partially embedded in the endometrial layer and myometrium.
(2) The IUD is completely incarcerated: the IUD is completely embedded in the myometrium or most of it is embedded in the myometrium and part of the uterine serosa is exposed.
(3) Ectopic IUD outside the uterus: The IUD is ectopic in the pelvic cavity, intraperitoneal cavity, bladder, bowel, broad ligament or extraperitoneal.
1 case
After giving birth to her second baby 6 years ago, Ms. Chen took an intrauterine ring for contraception. In the past two months, I have often felt pain in the lower abdomen, and occasionally there is a small amount of vaginal bleeding. Ms. Chen hurried to the hospital for a color Doppler ultrasound examination, and the results showed that the intrauterine ring was incarcerated in the muscle layer. That is to say, this birth control ring is restless and works hard, and it is stuck in the muscle layer of the uterus, which requires surgical treatment.
Feel the trouble of the situation. The doctor quickly arranged a hysteroscopy. Under the microscope, it can be seen that the arms of the "V"-shaped birth control ring are deeply inserted into the corneal muscle layer. This situation is very dangerous if ordinary ring removal is performed. , The pain of patients who fail to take the ring under the blind detection state increases, and the consequences of uterine perforation are very serious.
Therefore, the hysteroscopic ring removal was implemented, and the intrauterine situation was clear at a glance under direct vision, and the IUD was successfully and completely removed. The patient is not hospitalized, no surgery is required, and the procedure is basically pain-free. The operation time is only a few minutes, and the patient can leave the hospital immediately after the operation.
2 cases
The 60-year-old Aunt Liu has been menopausal for more than 10 years. When she was young, she placed an IUD in her uterus for contraception. In the past two weeks, Aunt Liu felt uncomfortable in her stomach, so she wanted to take out the IUD. After examination, it was found that Aunt Liu’s cervix had Atrophy, coupled with 2 cesarean sections, the uterus was densely adhered to the anterior abdominal wall, resulting in the cervix being invisible. If you can't see the cervix, you can't take the ring at all! This is equivalent to not being able to find the door and not being able to enter the house at all. This is sadly pregnant with Aunt Liu and her daughter. After discussion by doctors, this problem can be solved by hysteroscopic surgery! Under the direct vision of hysteroscope, the cervix was successfully found and entered the uterine cavity. It was found that Aunt Liu's IUD had been incarcerated in the flesh. With the assistance of hysteroscopy and ultrasound, the IUD was successfully removed in only 10 minutes. , solved the big problem that plagued Aunt Liu.
In this operation, the natural vaginal canal is used to achieve no incision and no scars. Using hysteroscopic endoscopic technology, the IUD can be successfully removed when the cervix is severely atrophied and cannot be exposed. It is really a "small palace". Endoscopy, solve big problems"! I would also like to remind female friends that if you have been menopausal for half a year, please take out the IUD as soon as possible, because the uterus shrinks after menopause, but the size of the IUD remains unchanged, resulting in the risk of ectopic and incarcerated IUDs. greatly increase!
Expert interpretation
In fact, it is not uncommon for Ms. Chen and Aunt Liu to have such a situation, which is medically called ectopic IUD.
01
What are the causes of ectopic IUDs?
1. Improper operation to put the IUD outside the uterine cavity.
2. The IUD is too large, too hard, or the uterine wall is thin and soft, and the uterine contraction causes the IUD to gradually ectopic to the outside of the uterine cavity.
02
Diagnosis of ectopic IUD?
When the IUD is not in the normal position in the uterine cavity, it is called ectopic IUD, including the downward movement, incarceration, and external movement of the IUD.
1. The sonographic image of the normal metal IUD position is a strong echo in the center of the endometrial cavity, and a hypoechoic halo around the endometrium. In addition, by measuring the distance between the upper edge of the IUD and the fundus of the uterus or the distance between the lower edge of the IUD and the internal uterine opening, it can be judged whether the position of the IUD is normal.
2. IUD descending indexing is mild: the upper edge of the IUD is less than 25mm away from the fundus serosal surface; moderate: the upper edge of the IUD is 25-35mm away from the fundus serosal surface; severe: the upper edge of the IUD is away from the fundus serosal surface >35mm.
3. The degree of IUD embedded in the myometrium is mild: the depth of the IUD embedded in the muscle wall is less than 1/3; moderate: the depth of the IUD embedded in the muscle wall is 1/3~2/3; severe: the depth of the IUD embedded in the muscle wall is > 2/3 or more Uterine serous surface.
03
How to prevent ectopic IUD?
First, choose a regular medical institution to place the IUD, and secondly, complete the preoperative examination to exclude genital malformations (such as septate uterus, double uterus, etc.), genital tumors (such as submucosal fibroids) and serious systemic diseases. At the same time, choose the appropriate type of IUD and place it within 3-7 days after the menstrual period is clean.
04
What precautions should be taken after placing the IUD?
1. Avoid heavy physical labor within 1 week after placement.
2. Do not take baths and have sex within 2 weeks.
3. Follow-up at 1, 3, 6, and 12 months in the first year after surgery, and once a year thereafter until discontinuation. See a doctor at any time in special circumstances.
4. Take out the birth control ring in time when the age of placement is reached.
05
Do I have to take out the IUD?
First of all, we should choose to know that the IUD also has a time limit. If it exceeds the service life, it is recommended to take it out in time regardless of the contraceptive effect or the occurrence of long-term complications.
For women within 1 year after menopause, there is no need for contraception, and the IUD needs to be removed in time. After menopause, the estrogen and progesterone in the body decrease significantly, the uterus shrinks, the cervix becomes tight, the myometrium becomes thinner, and the size of the IUD does not change, the shrunken uterus may be embedded in the uterine wall by the IUD, that is, the IUD is embedded. If it is embedded in the blood vessel, it may cause massive bleeding; if it travels in the abdominal cavity, it can cause a series of abdominal complications (abdominal pain, infection, etc.); Causes unexplained hematuria and other conditions (as in the case of Ms. Wang's ectopic birth control ring). No matter what kind of heterotopia, it can cause difficulty or failure to take the ring, and even need to do laparotomy to take out the IUD.
Older women will inevitably get sick, and some diseases require an MRI examination. Generally, an MRI cannot be done with an IUD. So, for women who use an IUD, since it's in, it needs to be taken out later. Don't take chances and feel that since you don't feel anything, just stay in the womb. When I really feel anything, I am afraid that I will go to war.
Therefore, remind women of childbearing age and perimenopausal women again to choose a regular hospital to place the correct type of IUD. The IUD has a time limit. When it expires or there is no need for contraception, please take out the IUD in time.
Twisted birth control ring under hysteroscopy
Case 1: Reproductive age, anti-adhesion after assisted reproductive hysteroscopy, O-ring twisted and twisted with tail wire
Case 2: Reproductive age, anti-adhesion after assisted reproductive hysteroscopy, O-ring with tail wire
Case 3: Childbearing age, anti-adhesion after assisted reproductive hysteroscopy, O-ring twisted and constricted
Case 4: Child-bearing age, anti-adhesion after assisted reproductive hysteroscopy, with twisted O-ring and tail wire
Case 5: Child-bearing age, anti-adhesion after assisted reproductive hysteroscopy, O-ring twisted and twisted with tail wire
Case 6: Childbearing age, anti-adhesion after assisted reproductive hysteroscopy, twisted O-ring with tail wire
Case 7: Child-bearing age, anti-adhesion after assisted reproductive hysteroscopy, with twisted incarcerated O-ring with tail wire
Case 8: Reproductive age, anti-adhesion after assisted reproductive hysteroscopy, with twisted O-ring and tail wire
Case 9: Child-bearing age, anti-adhesion after assisted reproductive hysteroscopy, the O-ring is twisted and constricted
Case 10: Reproductive age, anti-adhesion after assisted reproductive hysteroscopy, T-ring congested
Case 11: Childbearing age, anti-adhesion after assisted reproductive hysteroscopy, T-ring congested
Case 12: 36 years old, Anhuan for 3 years of contraception, B-ultrasound in the other hospital showed ring incarceration, hysteroscopy showed that the T-ring moved down and rotated vertically, and the transverse arm was incarcerated on the anterior and posterior walls of the lower segment of the uterine cavity (cesarean section incision). scar level)
Case 13: 53 years old, Anhuan for 29 years of contraception, amenorrhea for half a year, the O-ring is twisted and incarcerated and concave with the right corneal polyp
Case 14: 44 years old, Anhuan for 10 years of contraception, abnormal uterine bleeding, the U-shaped ring moved down and rotated vertically, and both arms were stuck on the anterior and posterior walls of the cervical canal
Case 15: 28 years old, 6-year contraceptive with an annulus, pregnancy with a ring and seeing fetal heart rate, pregnancy in the right uterine angle, vertical rotation and displacement of the V-ring
Case 16: 50 years old, 27 years of contraceptive with an ring, 1 year of menopause, failed to take the ring outside the hospital, uterine atrophy, sealing and adhesion of the middle and lower uterine cavity, the birth control ring is located in the myometrium of the anterior wall of the uterus, hysteroscopic incision of the myometrium , the large foreign body forceps took out the T-ring bracket, the copper sleeve on the ring arm was not seen
Case 17: Childbearing age, anti-adhesion after assisted reproductive hysteroscopy, twisted and incarcerated with tail wire
Case 18: Childbearing age, anti-adhesion after assisted reproductive hysteroscopy, O-ring incarceration
Case 19: 65 years old, Anhuan 30 years of contraception, 10 years of menopause, stenosis of the vaginal orifice, atrophy and stenosis of the external cervical orifice, adhesion of the internal cervical orifice, hysteroscopic separation and adhesion, O-ring constriction, traction deformation, complete removal
Case 20: 30 years old, Anhuan for 7 years of contraception, B-ultrasonography in the outer hospital showed that the ring was displaced, the removal of the ring in the outer hospital failed, the hysteroscopy showed that the U-shaped ring moved down, and the arms were incarcerated on both sides of the cervical canal
Case 21: 47 years old, Anhuan for 13 years of contraception, amenorrhea for 4 months, failed to take the ring in another hospital, hysteroscopy showed that one arm of the U-shaped ring was entrapped into the left corneal myometrium
Case 22: 45 years old, Anhuan for 14 years of contraception, B-ultrasound showed that the birth control ring was incarcerated, and the removal of the ring in the other hospital failed. Hysteroscopy showed that one arm of the V-ring was embedded in the right wall of the lower uterine cavity, and the other arm was pulled Pulled to the external os of the cervix
Case 23: 26 years old, Anhuan for 1 month to contraception, B-ultrasound in the other hospital showed incarceration of the birth control ring, the ring removal in the other hospital failed, the hysteroscopy showed that the U-shaped ring was rotated horizontally, and the two arms were stuck on both sides of the left fallopian tube opening.
Case 24: 48 years old, 15 years of contraception with an ring, B-ultrasound showed that the birth control ring was incarcerated, the ring moved down, the arms were incarcerated on both sides of the lower segment of the uterine cavity, and the incarceration on the left side was deep, 1.8 mm from the serosa surface
Case 25: 52 years old, Anhuan for 12 years of contraception, the IUD remained after the ring was taken in a foreign hospital, and the residual IUD was found by hysteroscopy
Case 26: 38 years old, failed twice in vitro, spontaneous pregnancy after 1 year, cesarean section delivery, decreased menstrual flow, diagnosis of intrauterine adhesions, hysteroscopic separation of adhesions, two balloons and ring placement at the same time
Case 27: At childbearing age, 2 O-rings were installed in a reproductive center to prevent adhesion after assisted reproductive hysteroscopy.
Case 28: 58 years old, 35-year-old contraceptive ring, inadvertently placed 2 rings during childbearing age, B-ultrasound showed that the birth control ring was abrupt, and the ring removal in the other hospital failed. Stenosis of the vaginal opening, atrophy and narrowing of the cervical orifice, sealing and adhesion of the lower segment of the uterine cavity, separation of the adhesions by hysteroscopy, and more yellow purulent fluid flowing out of the uterine cavity, see two O-rings, one of which is inserted into the myometrium
Case 29: 74 years old, 35 years of contraception with an annular ring (3 rings in 15 years), 20 years of menopause, 3 O-rings were removed by hysteroscopy.
Precautions before and after hysteroscopy
Preoperative:
1. Hysteroscopy is generally the best for 3-7 days after menstruation is clean.
2. No sexual life after menstruation or three days before surgery.
3. Preoperative examinations: leucorrhea routine, blood routine, coagulation function, four preoperative items, liver and kidney function, blood type identification, electrocardiogram.
Postoperatively:
1. Sexual life and tub bathing for 1 month after surgery.
2. Rest for at least 1 week after surgery.
3. Proper antibiotic treatment is given after surgery.
4. If there is more vaginal bleeding, come to the hospital for treatment at any time.
5. Come to the hospital 7 days after the operation to get the pathology report.
- Recommended news
- 【General Surgery Laparoscopy】Cholecystectomy
- Surgery Steps of Hysteroscopy for Intrauterine Adhesion
- [Otolaryngology Otoscopic Section] Excision of Cholesteatoma in the External Auditory Canal
- [Otolaryngology Nasal Endoscopy] How to Treat Recurrent Rhinitis
- [ENT Surgery: Nasal Endoscopy] Endoscopic Treatment of Nasal Polyps