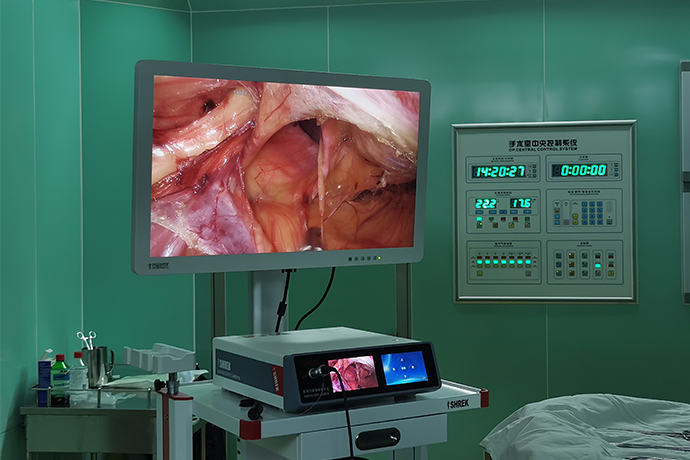
【Laparoscopy】Common Problems and Countermeasures When into the Abdomen
Release time: 01 Jun 2021 Author:Shrek
Endoscopic surgical instruments are different from traditional surgical instruments. Their product structure is relatively complex, with a wide variety of components and fine volume. Careful inspection and proper management are required during use. Improper operation can easily cause safety hazards, such as equipment damage, missing parts, or even Medical accidents can occur. This article introduces some common problems and countermeasures of abdominal laparoscopic surgery. I hope it will be helpful to all colleagues.
Loss of pneumoperitoneum
With the continuous development of laparoscopic surgery, laparoscopic surgery has been widely used clinically due to its advantages of less trauma, light pain, fast recovery, and less scars. Most laparoscopic surgery uses pneumoperitoneum, the most commonly used medium is C02. For those with cardiopulmonary insufficiency, helium (He) is also used as a distension material. In some cases, the established pneumoperitoneum may need to be temporarily released (eg, patient intolerance, hemodynamic instability, due to certain surgical procedures), or loss of gas due to channel leakage or equipment failure belly. Most trocars have a stopcock to easily release the pneumoperitoneum if needed. In order to re-establish the pneumoperitoneum, the cock can be turned back to conform to the airflow. To resolve accidental pressure loss, all possible locations for loss should be assessed, including air supply devices, inflation tubes, inflators, valves, and access ports (eg, peritoneal overtubes, leaks around trocars at the level of the fascia).
Surgical pain
After laparoscopic surgery, shoulder pain is common. This kind of pain is generally considered to be caused by irritation of the diaphragm (caused by fluid, blood, or carbonic acid produced by the mixture of carbon dioxide gas and water in the abdominal cavity) or the phrenic nerve being stretched during the operation.
The pain caused by trocar placement can be expected, but it can be minimized by using the following methods: use the minimum number of channels required for safe operation; minimize the number of large channels (ie ≥ 10mm); preoperative or at the end of the operation, a local anesthetic is injected into the channel. The main means to reduce the pain associated with abdominal ventilation is to reduce the initial inflation speed and inflation pressure. A systematic review identified 22 (n=1263) trials comparing low-pressure pneumoperitoneum with standard-pressure pneumoperitoneum for patients undergoing laparoscopic cholecystectomy. In 10 studies that reported this outcome, the low-pressure group had significantly lower pain scores and a lower incidence of shoulder pain. Between the low pressure group and the standard pressure group, no differences in the need to switch to open surgery or the incidence of complications were found to be clinically significant. Other methods include: CO2 heating and humidification; removal of residual CO2 at the end of the operation (this can be done by placing the patient in the trendelenburg position). The methods that can improve the discharge of retained CO2 include: perfusion of normal saline; use of lung recruitment method, which involves the need for anesthesiologists to perform multiple artificial lung expansions (increase intra-abdominal pressure).
Failed to enter the abdomen
If bile, intestinal contents, or blood flows back from the place where the veress needle is placed, the needle should be kept in place and an alternative abdominal access is immediately obtained. Laparoscopy can also be used as an alternative to the abdomen, unless significant bleeding occurs; in the case of significant bleeding, an open laparotomy is required. Any location where the abdomen fails should be checked to assess whether there is any related damage; if damage is found, appropriate repairs should be performed. If the abdomen fails but no complications occur, the abdomen can be tried again at the same location.
step:
●Estimate the length of the veress needle needed to enter the peritoneal cavity.
●Make a 5mm incision in the skin and subcutaneous tissue.
●Put the veress needle through the incision to the level of the fascia, mark the depth on the needle, and then pull out the needle.
●Grasp the fascia (for example, hand, Kocher forceps) and lift the abdominal wall. If it is under the costal arch, this step is not necessary. It is important to note that if only the skin is grasped without including the fascia when grasping, it may increase the failure rate of abdominal access.
●Hold the Veress needle, the holding position is close to the previously marked position, insert through the incision at a 45-degree angle, towards the pelvic cavity or away from the fixed organ, and be careful to avoid the veress needle from deviating to the side.
●Feel the sense of two breakthroughs. The first time was when the needle passed through the abdominal fascia, and the second time was when the needle passed through the mural peritoneum. When choosing a more lateral position to enter the abdomen, if you pass more than one layer of fascia, you may have an extra sense of breakthrough.
●When the needle enters the peritoneal cavity, the displaced needle connecting sleeve will make a “clicking sound” as the protective sheath bounces back to cover the end of the needle. The needle in the peritoneal cavity can also be compared with the needle in the abdominal wall, and move more freely.
When the needle enters the peritoneal cavity, the surgeon will usually feel the rebound of the protective needle sheath/needle core or hear a “click”, indicating that the resistance against the needle is no longer present. This click/rebound sensation usually indicates The Veress needle has entered the peritoneal cavity; however, if the needle of the Veress needle accidentally enters the hollow organ, this sound can also be felt, so one of several deterministic techniques should usually be used for confirmation before inflating through the needle.
Loss of casing position
If a channel slides in the abdominal wall, this channel may need to be reset and/or fixed by adding sutures. Even if the channel is not specifically designed to be sutured in situ (ie, without a retaining ring or suture), it can be easily secured by drainage or suture like a "shoelace". The use of longer or larger diameter trocars, or balloon/expandable head trocars can also help. Many Hasson trocars have an adjustable stopper, which can be fixed to various depths by a locking mechanism to prevent the channel from changing position.
Channel leak
If a channel or single-port device leaks during operation, it is usually because the fascia defect is too large or the channel angle is too large. Balloon tip trocars can help. Adding sutures or tightly clamping the tissue around the trocar with cloth pliers can also reduce leakage. Vaseline gauze can also be used to reduce the flow of any gas leakage.
Channel bleeding
The blood vessels of the abdominal wall can be injured during the abdominal operation. The position to enter the abdomen should be carefully chosen to avoid these blood vessels. Bleeding in the abdominal wall may not become obvious until the channel is removed, because the channel may fill up the muscle or bleed under the skin. In addition to checking for bleeding during the establishment of the abdomen port, the location of the abdomen should be inspected for bleeding during and after the removal of the channel. Bleeding points can usually be identified,and treated by electrocautery. Occasionally, it may be necessary to enlarge the skin incision to control bleeding. If the bleeding continues, you can also insert a Foley tube, inflate it, and gently pull it to fill the abdominal opening. If this operation fails, a U-shaped suture can be made to the abdominal wall through a suture passer and an absorbable braided suture under the direct view of the laparoscope. Care should be taken to suture the distal and proximal ends of the injured section of the blood vessel. Many special devices are designed to close the fascia of the passage opening, and these devices may also be useful for treating abdominal wall bleeding. Once bleeding occurs, the "four-step hemostasis method" can be applied to hemostasis. The author divides the steps of hemostasis operation into 4 parts: (1) Quickly control the bleeding point, which is temporary hemostasis. (2) Stabilize emotions and sort out ideas, determine the nature and location of bleeding, and formulate a hemostatic plan. (3) Clean up the blood in the operation field and dissect and separate the bleeding site to create conditions for definite hemostasis. (4) Deterministic hemostasis operation. In order to facilitate the memory, the formula of the four-step hemostasis method is summarized as: one clip, two stable, three clear, four confirmed.
Underexposure of the surgical field
If the visual field is exposed or anatomical separation is difficult or unsafe, additional trocars should be added to ensure the safety of the patient. This is especially important in single port surgery; If single port surgery can not get a good visual field, we should give up and choose multi-channel technology.Because the laparoscopic surgical instruments are not convenient for large-scale tissue stretch exposure, the most commonly used method of exposure is to change the body position and use the gravity effect to obtain the surgical view field.Normally, exposure by gravity is very effective, and the surgeon should make full use of it. However, there are some conditions that restrict the exposure of gravity, such as intestinal dilatation, intra-abdominal adhesions, and relatively small abdominal cavity volume. At this time, it is recommended to perform bowel decompression to loosen adhesions and deepen anesthesia. When changing the body position, you should also pay attention to the resulting cardiopulmonary burden, and you need to communicate with the anesthesiologist to avoid accidents. In addition, the patient's fixation must be reliable to avoid falling into the bed. Gravity exposure also facilitates the directional flow of liquid in the body cavity, which is conducive to cleaning the surgical view field. Some organs will obstruct the surgical field due to gravity. For example, the sagging uterus during rectal cancer surgery will obscure the pelvic cavity, and the drooping liver during gastric cancer surgery will affect the operation of the lesser curvature of the stomach. At this time, special traction hooks or sutures can be used. The hang improvement is revealed.
Extraperitoneal inflation
Subcutaneous, preperitoneal or omental inflation can occur in any abdominal technique. Some researchers suggest that directly entering the abdomen without inflation can minimize the incidence; but these data are limited. Any benefit of preventing incorrect inflation will be offset by the possibility of intestinal or vascular damage to the placement of the trocar before inflation. The Veress needle or Hasson trocar is initially confirmed to be placed in the peritoneal cavity. However, if the device is accidentally pulled out of the peritoneal cavity, subcutaneous CO2 insufflation will occur and the inflation pressure will quickly rise to 15mmHg or more. The abdominal wall will swell, but will not swell, and crepitus will be found in the subcutaneous tissue. Subcutaneous CO2 filling may increase end-tidal CO2. If extraperitoneal inflation has occurred, the anesthesiologist should be informed. Once the intraperitoneal inflation is completed, a small amount of extraperitoneal gas is usually quickly absorbed. For the elderly, as well as patients with impaired tissue integrity (such as collagen vascular disease or mixed connective tissue disease), subcutaneous CO2 inflation will progress rapidly and reach the chest wall, neck, and face quickly.

Loss of pneumoperitoneum
With the continuous development of laparoscopic surgery, laparoscopic surgery has been widely used clinically due to its advantages of less trauma, light pain, fast recovery, and less scars. Most laparoscopic surgery uses pneumoperitoneum, the most commonly used medium is C02. For those with cardiopulmonary insufficiency, helium (He) is also used as a distension material. In some cases, the established pneumoperitoneum may need to be temporarily released (eg, patient intolerance, hemodynamic instability, due to certain surgical procedures), or loss of gas due to channel leakage or equipment failure belly. Most trocars have a stopcock to easily release the pneumoperitoneum if needed. In order to re-establish the pneumoperitoneum, the cock can be turned back to conform to the airflow. To resolve accidental pressure loss, all possible locations for loss should be assessed, including air supply devices, inflation tubes, inflators, valves, and access ports (eg, peritoneal overtubes, leaks around trocars at the level of the fascia).
Surgical pain
After laparoscopic surgery, shoulder pain is common. This kind of pain is generally considered to be caused by irritation of the diaphragm (caused by fluid, blood, or carbonic acid produced by the mixture of carbon dioxide gas and water in the abdominal cavity) or the phrenic nerve being stretched during the operation.
The pain caused by trocar placement can be expected, but it can be minimized by using the following methods: use the minimum number of channels required for safe operation; minimize the number of large channels (ie ≥ 10mm); preoperative or at the end of the operation, a local anesthetic is injected into the channel. The main means to reduce the pain associated with abdominal ventilation is to reduce the initial inflation speed and inflation pressure. A systematic review identified 22 (n=1263) trials comparing low-pressure pneumoperitoneum with standard-pressure pneumoperitoneum for patients undergoing laparoscopic cholecystectomy. In 10 studies that reported this outcome, the low-pressure group had significantly lower pain scores and a lower incidence of shoulder pain. Between the low pressure group and the standard pressure group, no differences in the need to switch to open surgery or the incidence of complications were found to be clinically significant. Other methods include: CO2 heating and humidification; removal of residual CO2 at the end of the operation (this can be done by placing the patient in the trendelenburg position). The methods that can improve the discharge of retained CO2 include: perfusion of normal saline; use of lung recruitment method, which involves the need for anesthesiologists to perform multiple artificial lung expansions (increase intra-abdominal pressure).
Failed to enter the abdomen
If bile, intestinal contents, or blood flows back from the place where the veress needle is placed, the needle should be kept in place and an alternative abdominal access is immediately obtained. Laparoscopy can also be used as an alternative to the abdomen, unless significant bleeding occurs; in the case of significant bleeding, an open laparotomy is required. Any location where the abdomen fails should be checked to assess whether there is any related damage; if damage is found, appropriate repairs should be performed. If the abdomen fails but no complications occur, the abdomen can be tried again at the same location.
step:
●Estimate the length of the veress needle needed to enter the peritoneal cavity.
●Make a 5mm incision in the skin and subcutaneous tissue.
●Put the veress needle through the incision to the level of the fascia, mark the depth on the needle, and then pull out the needle.
●Grasp the fascia (for example, hand, Kocher forceps) and lift the abdominal wall. If it is under the costal arch, this step is not necessary. It is important to note that if only the skin is grasped without including the fascia when grasping, it may increase the failure rate of abdominal access.
●Hold the Veress needle, the holding position is close to the previously marked position, insert through the incision at a 45-degree angle, towards the pelvic cavity or away from the fixed organ, and be careful to avoid the veress needle from deviating to the side.
●Feel the sense of two breakthroughs. The first time was when the needle passed through the abdominal fascia, and the second time was when the needle passed through the mural peritoneum. When choosing a more lateral position to enter the abdomen, if you pass more than one layer of fascia, you may have an extra sense of breakthrough.
●When the needle enters the peritoneal cavity, the displaced needle connecting sleeve will make a “clicking sound” as the protective sheath bounces back to cover the end of the needle. The needle in the peritoneal cavity can also be compared with the needle in the abdominal wall, and move more freely.
When the needle enters the peritoneal cavity, the surgeon will usually feel the rebound of the protective needle sheath/needle core or hear a “click”, indicating that the resistance against the needle is no longer present. This click/rebound sensation usually indicates The Veress needle has entered the peritoneal cavity; however, if the needle of the Veress needle accidentally enters the hollow organ, this sound can also be felt, so one of several deterministic techniques should usually be used for confirmation before inflating through the needle.
Loss of casing position
If a channel slides in the abdominal wall, this channel may need to be reset and/or fixed by adding sutures. Even if the channel is not specifically designed to be sutured in situ (ie, without a retaining ring or suture), it can be easily secured by drainage or suture like a "shoelace". The use of longer or larger diameter trocars, or balloon/expandable head trocars can also help. Many Hasson trocars have an adjustable stopper, which can be fixed to various depths by a locking mechanism to prevent the channel from changing position.
Channel leak
If a channel or single-port device leaks during operation, it is usually because the fascia defect is too large or the channel angle is too large. Balloon tip trocars can help. Adding sutures or tightly clamping the tissue around the trocar with cloth pliers can also reduce leakage. Vaseline gauze can also be used to reduce the flow of any gas leakage.
Channel bleeding
The blood vessels of the abdominal wall can be injured during the abdominal operation. The position to enter the abdomen should be carefully chosen to avoid these blood vessels. Bleeding in the abdominal wall may not become obvious until the channel is removed, because the channel may fill up the muscle or bleed under the skin. In addition to checking for bleeding during the establishment of the abdomen port, the location of the abdomen should be inspected for bleeding during and after the removal of the channel. Bleeding points can usually be identified,and treated by electrocautery. Occasionally, it may be necessary to enlarge the skin incision to control bleeding. If the bleeding continues, you can also insert a Foley tube, inflate it, and gently pull it to fill the abdominal opening. If this operation fails, a U-shaped suture can be made to the abdominal wall through a suture passer and an absorbable braided suture under the direct view of the laparoscope. Care should be taken to suture the distal and proximal ends of the injured section of the blood vessel. Many special devices are designed to close the fascia of the passage opening, and these devices may also be useful for treating abdominal wall bleeding. Once bleeding occurs, the "four-step hemostasis method" can be applied to hemostasis. The author divides the steps of hemostasis operation into 4 parts: (1) Quickly control the bleeding point, which is temporary hemostasis. (2) Stabilize emotions and sort out ideas, determine the nature and location of bleeding, and formulate a hemostatic plan. (3) Clean up the blood in the operation field and dissect and separate the bleeding site to create conditions for definite hemostasis. (4) Deterministic hemostasis operation. In order to facilitate the memory, the formula of the four-step hemostasis method is summarized as: one clip, two stable, three clear, four confirmed.
Underexposure of the surgical field
If the visual field is exposed or anatomical separation is difficult or unsafe, additional trocars should be added to ensure the safety of the patient. This is especially important in single port surgery; If single port surgery can not get a good visual field, we should give up and choose multi-channel technology.Because the laparoscopic surgical instruments are not convenient for large-scale tissue stretch exposure, the most commonly used method of exposure is to change the body position and use the gravity effect to obtain the surgical view field.Normally, exposure by gravity is very effective, and the surgeon should make full use of it. However, there are some conditions that restrict the exposure of gravity, such as intestinal dilatation, intra-abdominal adhesions, and relatively small abdominal cavity volume. At this time, it is recommended to perform bowel decompression to loosen adhesions and deepen anesthesia. When changing the body position, you should also pay attention to the resulting cardiopulmonary burden, and you need to communicate with the anesthesiologist to avoid accidents. In addition, the patient's fixation must be reliable to avoid falling into the bed. Gravity exposure also facilitates the directional flow of liquid in the body cavity, which is conducive to cleaning the surgical view field. Some organs will obstruct the surgical field due to gravity. For example, the sagging uterus during rectal cancer surgery will obscure the pelvic cavity, and the drooping liver during gastric cancer surgery will affect the operation of the lesser curvature of the stomach. At this time, special traction hooks or sutures can be used. The hang improvement is revealed.
Extraperitoneal inflation
Subcutaneous, preperitoneal or omental inflation can occur in any abdominal technique. Some researchers suggest that directly entering the abdomen without inflation can minimize the incidence; but these data are limited. Any benefit of preventing incorrect inflation will be offset by the possibility of intestinal or vascular damage to the placement of the trocar before inflation. The Veress needle or Hasson trocar is initially confirmed to be placed in the peritoneal cavity. However, if the device is accidentally pulled out of the peritoneal cavity, subcutaneous CO2 insufflation will occur and the inflation pressure will quickly rise to 15mmHg or more. The abdominal wall will swell, but will not swell, and crepitus will be found in the subcutaneous tissue. Subcutaneous CO2 filling may increase end-tidal CO2. If extraperitoneal inflation has occurred, the anesthesiologist should be informed. Once the intraperitoneal inflation is completed, a small amount of extraperitoneal gas is usually quickly absorbed. For the elderly, as well as patients with impaired tissue integrity (such as collagen vascular disease or mixed connective tissue disease), subcutaneous CO2 inflation will progress rapidly and reach the chest wall, neck, and face quickly.

Previous
【Laparoscopy】Subtotal Hysterectomy
- Recommended news
- 【General Surgery Laparoscopy】Cholecystectomy
- Surgery Steps of Hysteroscopy for Intrauterine Adhesion
- [ENT Surgery: Nasal Endoscopy] Endoscopic Treatment of Nasal Polyps
- [Otolaryngology Nasal Endoscopy] Methods and Precautions for Nasal Bleeding Control under Nasal Endoscopy
- [Orthopedic UBE Section] Four Years of Evolution of UBE Technology: From Lumbar Fusion to the "Forbidden Zone" of Thoracic and Cervical Spine, and the Unignorable "Hydraulic Pressure Crisis"