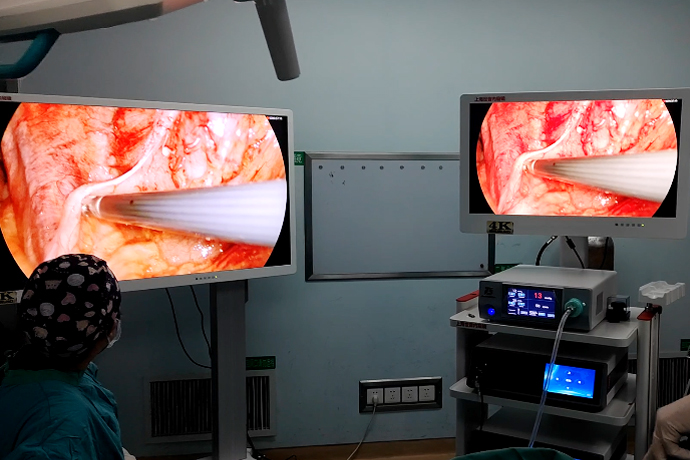
[General Surgery Laparoscopy] 4K ultra-high definition laparoscopic repair of gastric and duodenal perforation
Release time: 16 Apr 2024 Author:Shrek
Gastroduodenal perforation is one of the most common acute abdominal diseases in general surgery. It has a rapid onset and rapid progression. The most serious part is that a large amount of gastrointestinal fluid flows into the abdominal cavity after the perforation, causing chemical or bacterial peritonitis and even toxic shock. If not rescued in time, it can be life-threatening, so once diagnosed, surgical treatment is necessary.
Indications for repair of perforated gastric and duodenal ulcers:
1. The patient's general condition is poor, accompanied by shock or disease in important organs such as the heart, lungs, liver, kidneys, etc., and the peritonitis gradually becomes severe.
2. Those with complex perforation (such as cancer, bleeding, obstruction) or other suspected acute abdomen requiring immediate surgery.
3. Those with severe peritonitis, excessive abdominal effusion, severe intestinal paralysis, abdominal distension and obvious symptoms of poisoning.
4. After 6 to 12 hours of treatment according to the indications for non-surgical treatment (generally no more than 12 hours), the symptoms and signs are not relieved or worsened.
5. Those who are over 40 years old, have intractable ulcers with a long medical history, or are suspected of malignant gastric ulcers, or have perforation after eating, may consider surgical treatment.
Preoperative
History of ulcers (history of Helicobacter pylori infection), medication history (NSAIDS), and endoscopic history
History of current illness (typical abdominal pain), signs of peritonitis, blood test, CT (enhanced CT?)
Surgery (some operations only represent personal opinions)
1. Anesthesia:
Laparoscopic surgery under general anesthesia (if you can tolerate it); laparotomy surgery under local anesthesia (if you can’t tolerate it, haven’t tried it yet)
2. Posture:
Lying on the back with legs apart (living on the back to work), adducting the left hand (standing), abducting the right hand (administration), no need for a headrest (convenient for the hand holding the mirror to display the pelvic cavity), switching between head-up and head-down during the operation
3. Endoscopic system location and personnel positions:
The monitor, pneumoperitoneum and light source are placed on the upper right side of the patient; the main surgeon is on the left side of the patient, and the first assistant (mirror hand) is on the left side of the patient (caudal side of the main surgeon) or between the legs in a split-leg position, and the pelvic flushing is transferred to the right side of the main surgeon; the nurse is on The lower right side of the patient; it is better to hang the irrigation fluid on the upper right side of the patient
4. Equipment:
Endoscopic system, 3-hole method (10mm*2, 5mm*1) or 4-hole method (10mm*2, 5mm*2), negative pressure ball*2 or negative pressure ball*1+double cannula*1; needle holding device, suction device, non-destructive grasping forceps, separation forceps, scissors; 3-0 absorbable suture or 3-0 absorbable barbed wire, a pack of 1-0 silk thread, two corner needles
5.Punch location:
10mm observation hole at the lower edge of the umbilicus, 10mm main operating hole 2cm above the level of the umbilicus at the left midclavicular line (for surgical closure and placement of a pelvic drainage tube), 5mm auxiliary operating hole at the level of the umbilicus at the right midclavicular line (can be moved upward or outward as appropriate, surgical closure Venturi drainage tube)
If it is necessary to block the exposure of the liver, a 5mm auxiliary operating hole is placed 2cm below the ribs at the right midclavicular line.
6. Abdominal suction and exploration:
a. Is it perforated?
b. Gastric or duodenal perforation (pyloric ring location)?
c. Is there any pyloric obstruction or bleeding?
d. Perforation location, size, ulcer shape?
e. The direction of the longitudinal axis of the gastric antrum, pylorus, and duodenum (convenient for transverse sutures)?
Bacterial culture may be considered.
Gastric tube insufflation or methylene blue can be considered to help identify the lesion.
7. Repair and biopsy:
Biopsy of mucosal tissue should not be too small, and there is no need to force it (duodenal perforation may be malignant, consider the risk of stenosis; gastric perforation requires biopsy to rule out malignancy).
Determine the repair method (simple full-thickness repair + seromuscular embedding; simple full-thickness repair + pedicled omental coverage; pedicled omental coverage repair; pedicled omental filling).
Needle width, needle pitch (8-10mm, 3-5mm).
Suture choice (3-0 barbed suture or 3-0 microabsorbable suture).
Suture method (interrupted suture, continuous suture, figure-of-eight suture).
Omental flap cannot be performed in severe peritonitis, and round ligament flap is preferred.
8. Abdominal flushing and drainage:
The order of flushing (left subdiaphragm, infrahepatic recess, right subdiaphragm, right paracolic groove, small intestinal space, pelvic cavity, left paracolic groove).
According to the pollution situation, flush thoroughly: if the pollution is not serious, just rinse locally to avoid the spread of pollution; if the pollution is heavy, flush a large amount, generally no more than 3000ml (to avoid organ edema, increase anesthesia time, and affect the recovery of postoperative gastrointestinal function).
Indwelling drainage: 1 pelvic negative pressure bulb, 1 subhepatic recess negative pressure bulb or double cannula (elderly age, hypoalbuminemia, underlying diseases, repair, incision, and huge perforation, etc.).
Technique
Simple full-thickness repair +/- seromuscular embedding
Simple full-thickness repair + pedicled omentum coverage
Pedicled omentum coverage repair
Pedicled omental augmentation
Omental tamponade

- Recommended news
- 【General Surgery Laparoscopy】Cholecystectomy
- Surgery Steps of Hysteroscopy for Intrauterine Adhesion
- [Otolaryngology Nasal Endoscopy] How to Treat Recurrent Rhinitis
- [ENT Surgery: Nasal Endoscopy] Endoscopic Treatment of Nasal Polyps
- [Otolaryngology Nasal Endoscopy] Methods and Precautions for Nasal Bleeding Control under Nasal Endoscopy