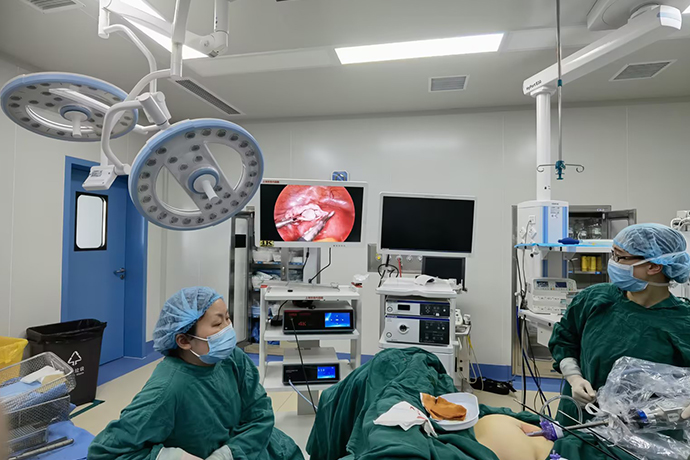
[Gynecological Laparoscopy] 4K laparoscopic recanalization after fallopian tube ligation
Release time: 26 Sep 2023 Author:Shrek
With the liberalization of the three-child policy, more and more women who have undergone fallopian tube ligation surgery have begun to think about having a third child. Fallopian tube ligation is a once-and-for-all method of contraception. Once ligated, it basically means that you cannot get pregnant again. However, things are unpredictable. After women undergo fallopian tube ligation surgery, they want to have another child due to various reasons, such as changes in marriage, accidents with their children, and the fully liberalized three-child birth policy. What to do at this time?
Can fertility be restored after sterilization?
The answer is yes! Fallopian tube recanalization helps women restore their reproductive functions.
Fallopian tube recanalization is to remove the fallopian tubes at the site of bilateral fallopian tube ligation or blockage, trim the two broken ends and reconnect them. The simple explanation is to connect the bridge of life where the egg and sperm meet so that the fertilized egg can pass through smoothly. .
In the past, due to the limitations of the family planning policy and contraceptive measures, a relatively large number of people had fallopian tube ligation in my country. In recent years, due to the relaxation of the national fertility policy, a larger number of patients after sterilization have the desire to have children again and hope to recover through surgery. The ability to conceive naturally. For young women, when there are no other infertility factors, considering the economic cost, pregnancy success rate, etc., fallopian tube ligation and recanalization should be the first choice.
What is the best surgical method to choose?
There are two surgical methods: laparotomy and laparoscopy. Compared with laparotomy, using 4K ultra-high-definition laparoscopy, doctors can see the surgical images very clearly on a large monitor screen, which reduces surgical risks, speeds up surgical time, and reduces patient trauma after surgery. It is small, with small postoperative scars, fewer complications, and fast recovery. It also improves the fallopian tube patency rate and pregnancy success rate after surgery.
Fallopian tube anastomosis is suitable for segmental fallopian tube resection or partial fallopian tube resection (after ligation). Surgically, there are 5 types of anastomosis, intermural-isthmus, intermural-ampullary, isthmus-isthmus, isthmus-ampullary and ampulla-ampullary.
First, a diagnostic laparoscopy was performed, and intraoperative fluid was passed through to determine whether the anastomosis was feasible. The standard is that there is at least 4cm of active fallopian tube, the proximal end of the fallopian tube is at least 3mm from the junction of the isthmus and interstitium, and the fimbriae end is open.
The proximal and distal ends of the fallopian tubes are removed. The opening of the fallopian tube is found under hysteroscopy, and then the 3F tube is inserted. The proximal and distal mesentery of the fallopian tube is sutured to bring the lumen closer. Suture the fallopian tube muscle layer with 6-0 absorbable suture to ensure that it does not penetrate the mucosa, grasp the muscle layer, and then tie the knot to tighten the proximal and distal ends.
The final anastomosis is completed after the intracavity knot is tied and tightened. The wound was closed with tissue glue and the guiding tube was removed under hysteroscopy. After confirming the patency of the lumen by passing fluid, the pelvic cavity is cleaned and flushed.
1. Routinely indwelling uterine cavity double-lumen fluid tube. Laparoscopic exploration of the pelvic and abdominal cavity, focusing on the site of fallopian tube ligation, the length and functional form of the remaining fallopian tube.
2. Hydraulic separation of the serosa layer of the fallopian tube at the ligation site: Use a No. 9 long puncture needle to inject pituitrin dilution (6U pituitrin + 0.9% NS20ml) into the subserosa of the fallopian tube on both sides of the ligation site to form a water cushion , while reducing bleeding, it can expand the serosal space and facilitate the separation of the fallopian tube core.
3. Use a monopolar electrocoagulation hook to make a vertical incision at the ligation scar and gradually separate the serosa layer (scissors can also be used to separate). When bleeding occurs, spot electrocoagulation will stop the bleeding. Preserve as much serosal tissue as possible to reduce tortuosity of the stylet core after anastomosis of the fallopian tubes.
4. Fully free ligation of the fallopian tube cores on both sides, cut off the ligation scar vertically, and retain as much normal fallopian tube tissue as possible. If the proximal fallopian tube core is narrower than the distal end, an appropriate oblique incision can be made to ensure that the anastomosis of the two fresh fallopian tube stumps is close in size.
5. Inject methylene blue liquid into the uterine cavity fluid tube to check whether the proximal end of the fallopian tube is unobstructed. Most patients with ligation have no abnormalities in the distal fallopian tube, so routine fluid inspection is not needed. If distal fallopian tube obstruction is suspected, a catheter can also be inserted. The stent is checked for fluid penetration.
6. Anastomize the broken ends of the fallopian tube: During the operation, 5-0 or 6-0 absorbable sutures are used to suture points 6, 12, 9, and 3 in sequence. The key points of suturing include: ① The first needle: Insert the needle from outside to inside at 6 o'clock on the proximal end of the fallopian tube, then take the needle out from the inside out at the distal end, suture through the wall of the tube, and tie the knot. The knot is located outside the fallopian tube cavity, leaving a length of about 3cm. The tail lines on both sides are placed at the 3 and 9 o'clock directions on both sides of the fallopian tube to assist in pulling and exposing the tube core. ②Second needle: Insert the needle from outside to inside at 12 o'clock at the distal end of the fallopian tube, and then take the needle out from inside to out at the proximal end, leaving a tail line about 3cm long for suspension and marking. For those with narrow stylets, the 12-point sutures should be left unknotted for the time being and kept in a loose state so that the various points of the stylet can be exposed and accurately positioned during subsequent suturing. ③The third needle: The main surgeon pulls the tail line at 12 o'clock, and the assistant pulls the suture line at 6 o'clock and leaves it in the direction of 3 o'clock, clearly exposing the walls of the two broken ends of the fallopian tube at 3 o'clock, suturing and tying. ④The fourth needle: similar to the method ③, pull and expose the tube wall at 9 o'clock and suture and tie it. If the lumen is larger, 1-2 more needles can be added appropriately.
7. Check the patency of the fallopian tube: Inject methylene blue solution, and see the smooth flow of methylene blue liquid from the fimbriae of the fallopian tube, which is the standard for patency. Observe whether there is obvious leakage at the anastomosis. If there is a lot of leakage at the anastomosis, continue to suture and reinforce it.
8. Use 4-0 absorbable sutures to intermittently suture the fallopian tube serosa layer with several needles to make the fallopian tube core smooth and not distorted. The surface of the serosa layer fully covers the fallopian tube core and is evenly aligned to reduce postoperative adhesions.
9. After anastomosing the contralateral fallopian tube with the same method, pass the fluid through again to check the patency of both sides of the fallopian tube.
Key points of surgical operation
(1) Hysteroscopy: Understand whether there are adhesions, vegetations, and abnormal uterine cavity development in the uterine cavity, and deal with them at the same time if necessary.
(2) Laparoscopic exploration: Exploring the pelvic cavity, checking the sites of bilateral fallopian tube ligation, and understanding whether there are any abnormalities in the uterus, ovaries, etc.
(3) Transvaginal fallopian tube drainage: Determine the condition of the isthmus of the fallopian tube. If the filling is good, you will see a blue filling sensation in the isthmus.
(4) Cut the surface mesangium of the fallopian tube at the proximal and distal ends of the fallopian tube ligation site to expose the fallopian tube core.
(5) Cut off the proximal and distal fallopian tube cores at the fallopian tube ligation site to expose fresh ports, cut off part of the fallopian tube at the ligation site, and use spot electrocoagulation to stop bleeding.
(6) Perform a fallopian tube patency with Meilan fluid to determine whether the proximal end of the fallopian tube is unobstructed: it can be seen that the Meilan fluid flows out smoothly.
(7) Perform end-to-end anastomosis on both sides: 5-0 absorbable sutures, interrupted sutures (note that the knots are tied outside the fallopian tube core), and 3-4 stitches a week.
(8) After the anastomosis, the fallopian tubes are drained with Meilan fluid to judge the effect of the fallopian tube anastomosis: If the anastomosis effect is good, it can be seen that the Meilan fluid flows out smoothly from the fimbral end of the fallopian tubes. There may also be fluid leakage from the fallopian tube anastomosis site, but no further treatment is required.
(9) Close the mesangium on the surface of the fallopian tube anastomosis with interrupted sutures.
(10) Carry out the fallopian tube anastomosis on the other side in the same way.
(11) After successful anastomosis on both sides, rinse the pelvic cavity repeatedly and cover the wound with an anti-adhesion membrane.
So what should you pay attention to after fallopian tube recanalization?
Some patients may experience some inflammation after fallopian tube recanalization. Antibiotics can be used for 3-5 days after the operation to prevent infection. At the same time, combined with our department's traditional Chinese medicine treatment, the pelvic microenvironment can be improved and infection and fallopian tube and pelvic adhesions can be prevented. Bathing in the tub is prohibited for one month after surgery. You should take rest in daily life, ensure adequate sleep, and engage in appropriate outdoor exercise to enhance your physical fitness. Once menstruation is delayed or there is a possibility of pregnancy after surgery, an early pregnancy test should be performed as soon as possible to determine whether there is intrauterine pregnancy.

- Recommended news
- 【General Surgery Laparoscopy】Cholecystectomy
- Surgery Steps of Hysteroscopy for Intrauterine Adhesion
- [Otolaryngology Nasal Endoscopy] How to Treat Recurrent Rhinitis
- [ENT Surgery: Nasal Endoscopy] Endoscopic Treatment of Nasal Polyps
- [Otolaryngology Nasal Endoscopy] Methods and Precautions for Nasal Bleeding Control under Nasal Endoscopy