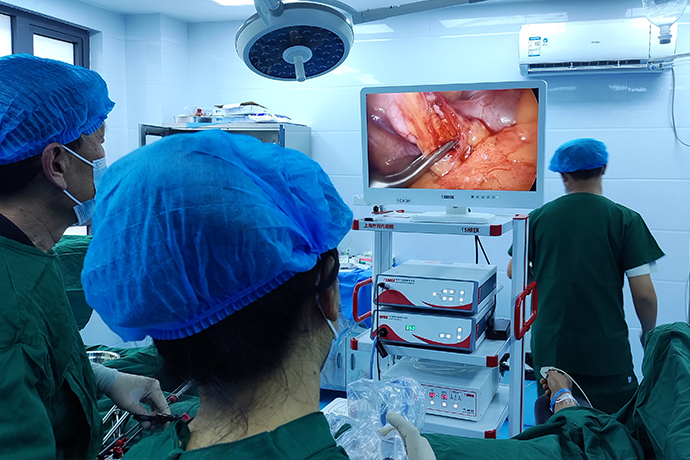
【Laparoscopy in Hepatobiliary Surgery】 Cholecystitis Surgery
Release time: 12 May 2023 Author:Shrek
For acute cholecystitis, which is better, laparoscopic surgery or open surgery, has been debated for many years. In the 1990s, LC was still a relative contraindication for acute cholecystitis. Later, with the rapid development of surgical techniques, surgical equipment, and optical equipment, the TG13 guideline believed that abdominal surgery is better than open surgery. Evidence-based medicine also believes that compared with open surgery, laparoscopic surgery has the advantages of fewer complications, shorter hospital stay (but no statistical difference), less incision pain, shorter hospital stay, faster recovery time, and higher quality of life. This article focuses on surgical techniques and describes the main points of LC in acute cholecystitis.
The main causes of cholecystitis are:
1. Biliary tract infection, and further development of biliary tract infection will cause gallbladder inflammation.
2. Intestinal parasitic diseases: For example, roundworms drill into the biliary tract and cause inflammation of the biliary tract.
3. Irregular meals, especially overeating, excessive consumption of high-fat and cholesterol-rich foods can easily lead to damage to the gallbladder and cause pathological changes.
4. In terms of mentality, long-term depression and poor emotions can easily lead to blocked bile excretion, and if things go on like this, they will also suffer from cholecystitis.
Indications for surgery
In principle, LC is indicated in cases of acute cholecystitis without previous epigastric surgery combined with omentum resection, Mirizzi syndrome or confluence of left and right hepatic duct stones. Although there is still debate about the period of LC surgery for acute cholecystitis, cholecystectomy should be performed in the early stage in the case of large stones incarcerated in the gallbladder neck and the first attack. For recurrent cases of cholecystitis, cases with abnormal liver function, or cases with prolonged onset, percutaneous hepatic gallbladder aspiration (PTGBA) or continuous drainage (PTGBD) can be performed first, and the procedure can be performed after the inflammation subsides (about 1 week). Cholangiography was performed to clarify the status of the cystic duct and common bile duct before LC.
Surgical field
Usually LC is performed under pneumoperitoneum. However, in acute cholecystitis, due to inflammation and edema, there may be more bleeding when separating the hepatoduodenal ligament and gallbladder bed. In addition, the part holding the gallbladder is prone to perforation, and bile leaks out, requiring constant suction. At this time, if the usual pneumoperitoneum is used, a good view cannot be guaranteed. Therefore, in acute cholecystitis LC, the method of subcutaneous puncture and abdominal wall suspension is often used, so that washing and suction can be performed like laparotomy. Usually in the case of acute cholecystitis, LC is the same as the preparation for laparotomy, and the laparotomy kit and additional sterile suspension instruments are routinely prepared.
Separation adhesion
In the initial episode of acute cholecystitis, the inflammatory adhesions around the gallbladder such as the greater omentum can be bluntly dissected in most cases. The oozing or small bleeding points on the separation surface can be naturally stopped by washing, etc., and can be burned with an electric knife without excessive hemostatic operations. For cases with a long time after onset and severe adhesions, a variety of hemostatic incision devices can be used to peel off along the gallbladder wall or retain a part of the gallbladder serosa to confirm that it has reached the Rouviere groove.
Intraoperative puncture and aspiration of gallbladder
It is difficult to control the inflamed gallbladder with high tension and thick wall. The gallbladder can be punctured with a special puncture needle through a 5mm Trocar first. When the wall is thick and hard, the gallbladder can be lifted with alligator-nose forceps with a large opening and strong grip.
Manipulation of the confluence of the cystic duct
The Rouviere groove is directly opposite the transition of the cystic duct and the neck of the gallbladder, and this is used as a target to determine the position of the cystic duct. When gallstones are incarcerated in the neck of the gallbladder, the Hartmann's capsule may be located at the right rear of the hepatic duodenum and produce adhesions. At this time, the neck of the gallbladder should be lifted to see the Rouviere groove clearly, and the adhesions should be separated from here.
As mentioned later, the gallbladder wall is swollen and hypertrophic in acute cholecystitis, which can be used to keep the outer layer of the gallbladder wall on the gallbladder bed like peeling a layer of onion (not the thin brown skin but the thicker white part) , so that the cystic duct and cystic artery can be identified and the procedure can be done safely. At this time, it is not only possible to use an electric knife for sharp dissection, but also to use a suction device to properly perform blunt dissection while sucking out the oozing blood. The cystic artery is identified by pulling the Hartmann's capsule down to the right. The cystic artery is cut first to facilitate the transcystic duct cholangiography before the cystic duct is cut, and it can also reduce intraoperative bleeding and maintain a clear field of view. At present, in order to minimize the legacy of titanium clips in the body, absorbable thread is used for in vivo or in vitro ligation of the cystic duct and cystic artery.
Intraoperative cholangiography
For cases with large stones incarcerated in the neck of the gallbladder, if there is no abnormal common bile duct in the preoperative imaging examination, and clear bile flows out from the broken end of the common bile duct when the cystic duct is incised, cholangiography may not be performed at this time. When there are small stones incarcerated in the cystic duct or purulent bile flows out from the broken end of the common bile duct, the cystic duct should be further carefully separated to the confluence of the three ducts, the cystic duct should be incised, the small stones or biliary sludge in the cystic duct should be squeezed out, and then open A catheter was inserted for cholangiography.
Separation of the gallbladder bed
When separating the gallbladder bed in acute cholecystitis, the level of separation should not be mistaken. The old surgical charts all recorded that before the separation of the gallbladder bed, normal saline or lidocaine was injected into the gallbladder wall to form artificial edema, so as to facilitate the separation of the gallbladder bed. In acute cholecystitis, the gallbladder wall has just been edematous, and it is important to preserve part of the gallbladder wall on the liver side. It is necessary not only to start the separation from the porta hepatis or the neck of the gallbladder, but also to make proper separation from the bottom, left and right sides of the gallbladder. After finding an appropriate separation level, continue the separation on this level. When no proper separation layer is found, the separation should be carried out as close to the gallbladder as possible consciously, and the deep surface of the liver side must not be cut. The detached instrument is not only electrocautery, but also powered Maryland forceps, suction, ultrasonic scalpel and Ligasure.
Take out the specimen
The gallbladder may be perforated and torn due to grasping and traction during puncture, suction or separation. In most cases, the excised gallbladder specimen has been destroyed. At this time, the gallbladder should be put into a specimen collector such as rubber gloves to protect the abdominal wall poking wound, and then taken out of the body.
Wash the wound and place a drainage tube
Usually, the patient's position is adjusted to a horizontal position or the head is slightly lowered, and the wound is washed with heparin saline until the fluid in the abdominal cavity is clear. When there is purulent bile leakage or heavy bleeding, change the position and wash the lower abdomen. After rinsing, it was confirmed that there was no bleeding and bile leakage.
Then a thin Penrose drainage tube was placed at the Winslow orifice.
Clinical Manifestations of Cholecystitis
1. Abdominal pain Patients with cholecystitis About 85% of patients with acute cholecystitis have pain in the right upper quadrant as the main symptom. Recurrent, mostly dull pain, distending pain.
2. Fever The fever in acute cholecystitis is generally 38-39°C, mostly without chills.
3. Nausea and vomiting are more common in acute cholecystitis.
4. Indigestion symptoms such as abdominal distension, belching and greasy feeling can occur in patients with acute and chronic cholecystitis, but chronic cholecystitis is more common.
5. Jaundice About 10% of patients with acute cholecystitis may develop mild jaundice, which may be caused by spasm of the sphincter at the lower end of the common bile duct or the spread of infection to the biliary system.

- Recommended news
- 【General Surgery Laparoscopy】Cholecystectomy
- Surgery Steps of Hysteroscopy for Intrauterine Adhesion
- [Laryngoscopy in Otolaryngology] Tonsillectomy
- [Otolaryngology Otoscopic Section] Excision of Cholesteatoma in the External Auditory Canal
- [Otolaryngology Nasal Endoscopy] How to Treat Recurrent Rhinitis