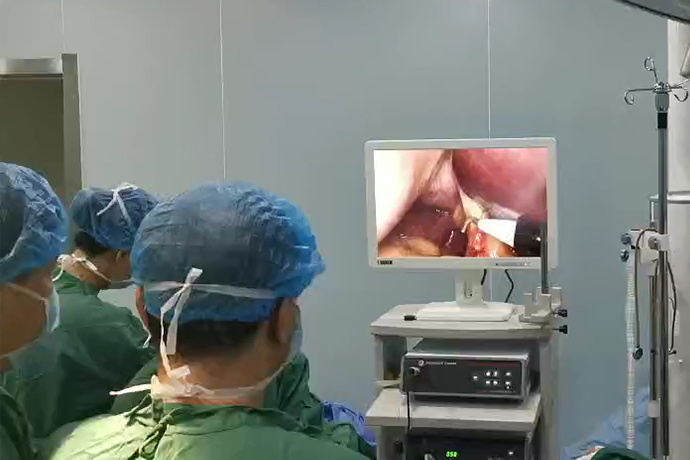
[Laparoscopic Hepatobiliary Surgery] Resection of hilar cholangiocarcinoma
Release time: 14 Feb 2023 Author:Shrek
Hilar cholangiocarcinoma is a common malignant tumor of the biliary system, and it is also a common malignant tumor. Because cholangiocarcinoma is hidden deep in the body, its onset is hidden, and its malignancy is high. Because of its special location, infiltrative growth, and close relationship with hilar blood vessels, surgical resection is extremely difficult. Radical resection of hilar cholangiocarcinoma is also considered the "peak" of the hepatobiliary profession.

The total laparoscopic radical resection of cholangiocarcinoma is even more difficult for surgeons. The complexity of hilar cholangiocarcinoma surgery is based on the complex local anatomy, and the progress of its surgery is based on the continuous in-depth and accurate understanding of the hepatobiliary and pancreatic anatomy.
The bile duct is a long, thin tube that carries the bile needed for the digestive process to help digest food. Cholangiocarcinoma is a malignant tumor originating from the bile duct epithelium. Intrahepatic cholangiocarcinoma is included in the category of "liver cancer", which has been introduced in previous articles. Cholangiocarcinoma occurs mostly in the age group of 20-70, with slightly more men than women, and the incidence rate has shown a clear upward trend in recent years. So, what are the symptoms of this disease?
The clinical manifestations of cholangiocarcinoma are related to its location and degree of bile duct obstruction. According to the anatomical site, cholangiocarcinoma is divided into hilar cholangiocarcinoma and lower cholangiocarcinoma, of which hilar cholangiocarcinoma accounts for about 2/3.
For hilar and extrahepatic cholangiocarcinoma, the tumor blocks the hilar bile duct and common bile duct, seriously affecting bile excretion, so jaundice can appear in the early stage, manifested as yellow staining of skin and sclera, yellow urine, skin itching and other symptoms. In addition, varying degrees of pain in the right upper abdomen is also a common symptom of cholangiocarcinoma, which is easily confused with symptoms of stomach problems, cholecystitis and other diseases. Fatigue, weight loss, and loss of appetite are common clinical symptoms of cholangiocarcinoma as a malignant tumor.
Why do you get cholangiocarcinoma? How did it develop?
In fact, the specific mechanism of cholangiocarcinoma has not been studied clearly, but there are some risk factors, such as bile duct inflammation, bile duct stones, bile duct parasites, etc. By quitting smoking, drinking and preventing gallstones and biliary tract infection, the risk of developing the disease can be reduced.
Cholangiocarcinoma is difficult to diagnose clearly based on clinical manifestations, and laboratory tests (such as elevated bilirubin, elevated serum tumor markers, etc.) and imaging examinations (CT, MRI, etc.) are often needed to further confirm the diagnosis.
First porta hepatis:
The main structures entering and exiting the first hilum are the portal vein, hepatic artery, and the extrahepatic biliary system. The understanding of the first hepatic hilum is mainly the understanding of the relationship between the three vessels, which is the center of the surgery for hilar cholangiocarcinoma. The three tubes are wrapped around the hepatoduodenal ligament to form the hepatic pedicle, and the dissection of the hepatoduodenal ligament lymph nodes is based on an accurate understanding of the relationship between the three tubes.
Serves as a key pathway for hepatic blood flow. The first porta hepatis is also a key site for hepatectomy to control bleeding. Pringle's maneuver was proposed by James Hogarth Pringle (1863-1941) in 1908. It controls the hepatoduodenal ligament through non-invasive clamping and placing blocking bands to reduce the entry of the hepatic artery and portal vein into the liver. Blood flow, which reduces bleeding during liver resection surgery, is fundamental to liver surgery. However, the liver resection for hilar cholangiocarcinoma is mostly regular liver resection, and at the same time when the hepatoduodenal ligament is skeletalized, the artery and portal vein to be hemihepatic resection are ligated and cut off respectively. In this way, when the liver is cut It is rare to block the portal of the liver anymore. Therefore, this method is not commonly used.
Second and third hepatic portals
The second hepatic porta and the third hepatic porta are the outflow channels of blood flow in the liver. The left, middle, and right hepatic veins return to the superior and inferior hepatic veins to form the second porta hepatis, and the other short hepatic veins returning to the retrohepatic inferior vena cava form the third porta hepatis, with 3-4 short hepatic veins at least and more 7-8 lines are the key parts of the free caudate lobe of the liver, among which the large right posterior inferior hepatic vein and right posterior middle vein are of great significance in irregular hepatectomy.
Several landmark anatomical structures closely related to the second hilum:
1: Makuuchi ligament (Makuuchi ligament): also known as the vena cava ligament, is a thin layer of connective tissue or liver tissue surrounding the right retrohepatic inferior vena cava near the second hepatic hilum. Located in the upper third of the retrohepatic inferior vena cava, it starts from the right lobe of the liver, bypasses the right and posterior walls of the retrohepatic inferior vena cava, and connects to the left wall and the left caudate lobe. The width is 0.5-3.0cm, and there may be small short hepatic veins in it, which need to be ligated during treatment. After cutting this ligament, the right wall of the right hepatic vein and its lower border can be clearly exposed, so as to facilitate further operations related to the right hepatic vein.
2: Hepatic vena cava space (fossa): It is a depression surrounded by the left wall of the right hepatic vein, the anterior wall of the vena cava, the right wall of the middle hepatic vein (left CCM), and the surface of the vena cava of the liver. It can be visualized after cutting the left and right coronary ligaments and dissecting the superior and inferior hepatic vena cava. There are few short hepatic veins in it, which is the only way to dissect the hepatic veins.
3: The space between the left CCM and the inferior vena cava: it is a potential gap between the posterior wall of the left CCM and the anterior wall of the vena cava. From the left hepatic vein to the lower border of the left wall of the inferior vena cava, and finally to the space of the hepatic vena cava, the width is equivalent to the width of the left CCM. It is easier to dissect out this gap after cutting off the cephalic end of the venous ligament, and free the left CCM.
In recent years, with the development of minimally invasive techniques and the continuous updating of surgical concepts, the feasibility, safety, and short-term therapeutic effects of laparoscopic hilar cholangiocarcinoma radical resection have gradually been recognized by some domestic experts. In order to standardize clinical diagnosis and treatment, ensure patient safety and improve prognosis, the laparoscopic hilar cholangiocarcinoma operation specification expert group and the editorial department of Chinese Journal of Surgery organized relevant domestic experts to follow the principles of hilar cholangiocarcinoma treatment and laparoscopic operation Technical specifications, formulating expert recommendations for laparoscopic radical resection of hilar cholangiocarcinoma.
Surgical steps
1. Abdominal exploration
2. Separation of the round ligament and falciform ligament
3. Free gallbladder
4. Cut off the common bile duct and send the margin for examination
5. Pull out the proper hepatic artery
6. Vascular skeletalization, lymph node dissection
7. Isolation of the gallbladder
8. Cut off the left hepatic artery and the left branch of the portal vein, and suture and reinforce them
9. Cut off the junction of the bile ducts in the anterior and posterior lobes of the right liver, and send the resection margins for examination
10. Free Left Liver
11. Mark the ischemic line with electric hook
12. Placement of hilar blockade
13. Free excision of spiegel leaves
14. Cut the liver along the ischemic line and the middle hepatic vein
15. Cut off the left hepatic vein with the closer
16. Middle hepatic vein suture reinforcement
17. Severing the jejunum by cutting the closer
18. Free jejunum and mesenteric vessels
19. Open the transverse mesocolon
20. Gallbladder anastomosis
21. Place the T-tube
22. Intestinal anastomosis
23. Closing the mesangial hole
24. Place the drainage tube
Indications and contraindications The indications for laparoscopic radical resection of hilar cholangiocarcinoma are more stringent. Preoperative CT, MRCP, CT angiography or magnetic resonance angiography should be combined to clarify the relationship between the tumor and the hepatic artery and portal vein and whether there is invasion. The indications include Bismuth-Corlette type I, II, some types III and some IV Type (without portal vein and hepatic artery violation). Contraindications include all contraindications for open radical resection of hilar cholangiocarcinoma, including those who cannot tolerate pneumoperitoneum or cannot establish pneumoperitoneum, and those with extensive abdominal adhesions or lesions that are difficult to expose and separate; tumors that invade the portal vein or Patients with the main hepatic artery; patients with difficulty in laparoscopic exposure, or patients with regional portal hypertension in the hepatic hilum who cannot safely undergo radical resection of the tumor.
- Recommended news
- 【General Surgery Laparoscopy】Cholecystectomy
- Surgery Steps of Hysteroscopy for Intrauterine Adhesion
- [Otolaryngology Otoscopic Section] Excision of Cholesteatoma in the External Auditory Canal
- [Otolaryngology Nasal Endoscopy] How to Treat Recurrent Rhinitis
- [ENT Surgery: Nasal Endoscopy] Endoscopic Treatment of Nasal Polyps