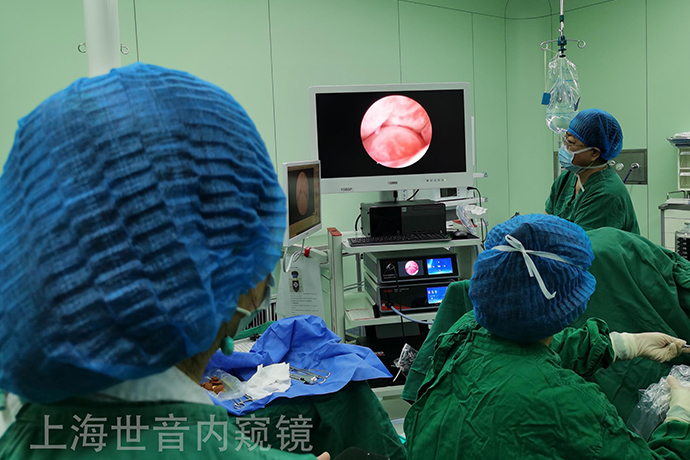
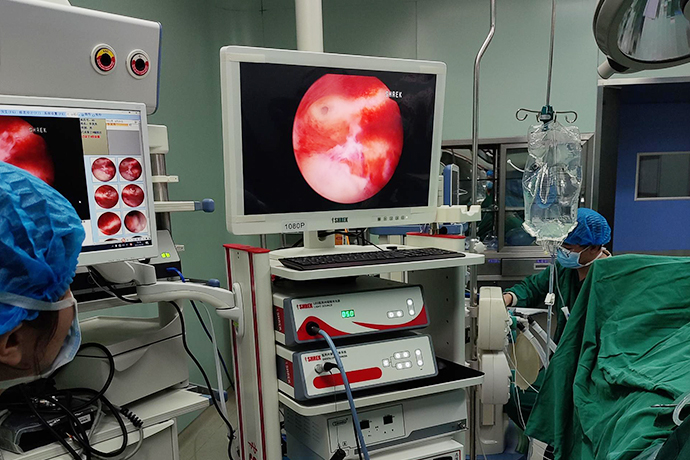
[Gynecological hysteroscopy] Abnormal hysteroscopy and surgery
Release time: 19 Oct 2022 Author:Shrek
Causes of abnormal uterine bleeding
Abnormal Uterine Bleeding (AUB): defined as heavy bleeding, irregular bleeding, and abnormal menstrual bleeding. The incidence of AUB in the population: 11%-13% (36-40 years old: 24%), common symptoms in gynecological outpatient clinics, and main indications for hysteroscopy. The main causes are as follows:
1. Endometrial polyps
2. Submucosal uterine fibroids
3. Adenomyosis/disease
4. Intimal hyperplasia/endometrial hyperplasia
5. Endometrial cancer
6. Ovulation disorders: Dysfunctional Uterine Bleeding (DUB), mostly endocrine diseases (PCOS, hyperprolactinemia, hypothyroidism, mental stress, obesity, anorexia, weight loss, excessive exercise, etc.)
7. Endometrial inflammation: menopause, separation of the uterine cavity, a small amount of secretions
8. Coagulation disorders
9. Iatrogenic: "BreakthroughBleeding", IUDs (Mirena), anticoagulants (warfarin, heparin)
10. Uncategorized: cesarean section scar/diverticulum, chronic endometritis, arteriovenous malformation, uterine muscle hypertrophy
However, these diseases do not all exist independently, and some patients may coexist with several diseases at the same time, causing AUB together.
Cooperating with hysteroscopy and treatment is a minimally invasive diagnosis and treatment technology, and its advantages are obvious: 1. Multi-angle examination, intuitive effect, no missed diagnosis; 2. No incision, fast recovery; 3. Short hospital stay; Professional doctors can complete the treatment in a short time without affecting normal physiological functions, and can return to normal work and life after surgery; 4. The operation is minimally invasive, with less medication and low cost, reducing the burden on patients.
Below we learn more about it.
endometrial polyps
It accounts for 21%-39% of the entire AUB cause. Endometrial polyps are one of the common benign endometrial lesions. They are localized hyperplasia of the basal layer of the endometrium, which is caused by the formation of a pedicle protruding into the uterine cavity. It belongs to the category of chronic endometritis and is prone to recurrence.
1. Symptoms
Symptomatic patients (70%-90%) mainly have irregular vaginal bleeding (increased menstrual flow, prolonged menstrual period, intermenstrual bleeding, and postmenopausal vaginal bleeding) and infertility. A small number of leucorrhea increased, bloody leucorrhea as the main performance. About 30% of patients still have no obvious clinical symptoms.
2. Good hair people
Women over 35 years of age, and those with the following medical conditions: adenomyosis, cervical polyps, diabetes, obesity, hypertension, endometritis, endometriosis, uterine fibroids, and tamoxifen use women etc.
3. Diagnosis
It can usually be found by pelvic ultrasonography, and the best time to check is before the 10th day of the menstrual cycle. The diagnosis needs to be removed under hysteroscopy for pathological examination.
4. Treatment
For functional endometrial polyps with a diameter of less than 1 cm, if asymptomatic, the spontaneous disappearance rate within 1 year is about 27%, and the malignant transformation rate is low, and follow-up can be observed. For symptomatic endometrial polyps larger than 1 cm, treatment is recommended. There are many treatment methods. Hysteroscopy is considered to be the best choice for the diagnosis and treatment of endometrial polyps.
It is especially suitable for those who are not pregnant or still have pregnancy requirements, as well as those who have various medical complications in the elderly; the risk of recurrence after endometrial polyps is about 3.7%-10.0%, and combined drug therapy after hysteroscopic polyp resection is to prevent its recurrence. key.
Adenomyosis
Adenomyosis is a condition in which endometrial glands or stroma are ectopic in the myometrium, accompanied by hyperplasia and hypertrophy of surrounding myometrium cells, forming diffuse or localized lesions.
The reported incidence of adenomyosis in China is 13.4%, and the reported incidence in foreign countries ranges from 5% to 70%, and there is a rising trend. It has become a common gynecological disease.
It mostly occurs in multiparous women aged 30-50, and in recent years, adenomyosis has shown an obvious trend of rising incidence and younger age of onset.
About 15% have endometriosis at the same time, and about 50% have uterine fibroids.
uterine leiomyoma
About 20% of adult women will have different types of uterine fibroids in their lifetime. According to the growth site, uterine leiomyomas can be divided into submucosal fibroids that affect the shape of the uterine cavity and other fibroids. The former is most likely to cause AUB.
1. Symptoms
Increased menstrual volume, prolonged menstrual period, severe anemia may occur secondary to symptoms such as fatigue and palpitations. When submucosal fibroids are accompanied by necrotic infection, there may be irregular vaginal bleeding or bloody purulent discharge, while fibroids (hyalinizing, cystic, erythroid, sarcomatoid, calcified) may appear Pain and other symptoms, in addition, can also cause infertility, miscarriage and so on.
2. Diagnosis
Usually, it can be found by pelvic ultrasound, hysteroscopy, laparoscopy, MRI, etc., and the diagnosis can be confirmed by postoperative pathological examination.
3. Treatment
Conservative treatment is suitable for asymptomatic patients, especially women near menopause, and can be followed up every 3-6 months.
Drug therapy is suitable for patients with mild symptoms, near-menopausal age or general conditions who are not suitable for surgery. Surgical treatment is suitable for patients with secondary anemia caused by menorrhagia and ineffective drug treatment; severe abdominal pain; large volume or affecting the bladder, rectum and other compression symptoms; suspected malignant transformation; it can be determined that submucosal fibroids are the only cause of infertility or miscarriage By.
Hysteroscopic electrical myomectomy (TCRM) is considered the modality of choice for the treatment of submucosal uterine fibroids.
Hysteroscopic endometrial ablation is indicated for patients with heavy menstrual flow and no fertility requirements but who wish to preserve the uterus or who cannot tolerate hysterectomy.
If fibroids are found after pregnancy, they tend to be treated conservatively, and surgical treatment is generally not recommended.
Endometrial malignancy and dysplasia
Atypical endometrial hyperplasia and malignant transformation are rare but important causes of AUB. Atypical endometrial hyperplasia is a precancerous lesion, with a cancer rate of 8% to 29% after 13.4 years of follow-up.
Common in patients with polycystic ovary syndrome (PCOS), obesity, tamoxifen use, and occasionally in ovulatory patients with luteal insufficiency.
1. Symptoms
Irregular uterine bleeding, which may alternate with oligomenorrhea. A few manifested as intermenstrual bleeding, and patients were often infertile.
2. Diagnosis
Endometrial biopsy is required to confirm the diagnosis.
Those who are aged ≥45 years, have long-term irregular uterine bleeding, have high-risk factors for endometrial cancer (such as hypertension, obesity, diabetes, etc.), have excessive thickening of the endometrium with uneven echoes indicated by B-ultrasound, and have no significant effect of drug treatment, should Diagnosis and curettage and pathological examination are performed, and biopsy under direct vision hysteroscopy is preferred for those with conditions.
3. Treatment
The treatment of atypical endometrial hyperplasia requires different treatment options according to the severity of endometrial lesions, the age of the patient and the need for fertility. Hysterectomy is recommended for patients >40 years of age with no reproductive requirements.
For young patients with fertility requirements, after comprehensive evaluation and adequate consultation, endometrial atrophy can be treated with a full cycle of continuous high-efficiency synthetic progesterone, such as medroxyprogesterone, megestrol, etc. After 3 to 6 months Line diagnosis and curettage plus suction (in order to achieve the purpose of comprehensive sampling).
If the endometrial lesions are not reversed, the dose should be continued to be increased, and reexamination should be performed after 3 to 6 months. If the atypical endometrial hyperplasia disappears, assisted reproductive technology treatment should be actively given after discontinuation of progesterone.
At the same time of using progesterone, high-risk factors for endometrial hyperplasia, such as obesity and insulin resistance, should be treated at the same time. The diagnosis and treatment of endometrial malignancies refer to relevant clinical guidelines.
Systemic coagulation-related diseases
Including aplastic anemia, various types of leukemia, various coagulation factor abnormalities, thrombocytopenia caused by various reasons and other systemic coagulation abnormalities.
It has been reported that about 13% of women with menorrhagia have systemic coagulation abnormalities.
1. Symptoms
Menorrhagia, intermenstrual bleeding, or prolonged menstrual periods. There are also other parts of the bleeding tendency (skin, mucous membranes, joints, muscles, etc.), severe cases may appear anemia, fever and other symptoms.
2. Diagnosis
Patients who are positive for any of the following 3 items suggest possible coagulation abnormalities and should consult a hematologist, including:
Menarche and menorrhagia.
History of 1 of the following: Past postpartum, post-surgical, or dental procedure-related bleeding.
Two or more of the following symptoms: bruising 1 to 2 times a month, nosebleeds 1 to 2 times a month, frequent gum bleeding, and a family history of bleeding tendencies.
3. Treatment
It should be negotiated with the Department of Hematology and other related departments. In principle, the treatment measures of the Department of Hematology should be the main treatment measures, and the Department of Gynecology should assist in the control of menstrual bleeding.
Drug therapy is the first choice for gynecology. The main measures are the treatment of endometrial atrophy with high-dose synthetic progesterone, and sometimes testosterone propionate is added to reduce pelvic organ congestion.
Tranexamic acid, short-acting oral contraceptives may also help. When the drug treatment fails or the primary disease has no cure, surgery can be considered to control the disease and improve the general condition in the hematology department.
Surgical treatment includes endometrial ablation and total hysterectomy.
Ovulation disorders
Ovulation disorders include oligoovulation, anovulation and luteal insufficiency, mainly caused by abnormal hypothalamic-pituitary-ovarian axis function, common in adolescence, menopause transition period, and reproductive period can also be caused by PCOS, obesity, hyperprolactinemia, Thyroid disease, etc.
1. Symptoms
Often manifested as irregular menstruation, menstrual volume, menstrual length, cycle frequency, regularity can be abnormal, sometimes causing heavy bleeding and severe anemia.
2. Diagnosis
The most commonly used methods for anovulation are basal body temperature (BBT) and mid-luteal blood progesterone levels. Ultrasound monitoring, etc.
3. Treatment
The principle is to stop bleeding and correct anemia during the bleeding period, adjust the cycle after the bleeding stops to prevent endometrial hyperplasia and AUB recurrence, and stimulate ovulation for those with fertility requirements.
Methods of hemostasis include progesterone endometrial shedding, high-dose estrogen endometrial repair, short-acting oral contraceptives or high-efficiency synthetic progesterone endometrial atrophy, and curettage.
The method of adjusting the cycle is mainly progesterone therapy in the second half of the period. Patients of puberty and reproductive age should choose natural or near-natural progesterone (such as dydrogesterone), which is conducive to the establishment or recovery of ovarian axis function.
Short-acting oral contraceptives are mainly suitable for women who require contraception. LNG-IUS can be placed for those who have completed childbirth or who have not had a childbearing plan for nearly 1 year, which can reduce the amount of bleeding in anovulatory patients and prevent endometrial hyperplasia.
Endometrial ablation or hysterectomy may be considered in patients who have completed fertility, have failed medical therapy, or have contraindications. Ovulation induction therapy is suitable for anovulatory patients with fertility requirements, and AUB can be corrected at the same time, depending on the cause of anovulation.
Endometrial local abnormality
When AUB occurs in a regular and ovulatory cycle, especially when no other reasons can be found after investigation, it may be caused by local abnormalities in the endometrium.
1. Symptoms
Menorrhagia, intermenstrual bleeding, or prolonged periods.
2. Diagnosis
At present, there is no specific method for diagnosing local endometrial abnormalities, which is mainly determined after excluding other definite abnormalities on the basis of ovulatory menstruation.
3. Treatment
For menorrhagia caused by such non-organic diseases, drug treatment is recommended first. The recommended order of drug treatment is:
LGIUS, suitable for those who have no fertility requirements for more than 1 year.
Tranexamic acid antifibrinolytic therapy or non-steroidal anti-inflammatory drugs (NSAIDs) can be used for those who are unwilling or unable to use sex hormone therapy or who want to conceive as soon as possible.
Short-acting oral contraceptives.
Progesterone endometrial atrophy treatment, such as norethisterone 5mg 3 times a day, starting from the 5th day of the cycle, taking it continuously for 21d. Dilation and curettage is only used for emergency hemostasis and pathological examination. For those without fertility requirements, conservative surgery, such as endometrial ablation, may be considered.
iatrogenic AUB
It refers to AUB caused by factors such as the use of sex hormones, the placement of an intrauterine device, or traditional Chinese medicine health products that may contain estrogen.
Withdrawal bleeding caused by the missed dose of contraceptives, if the amount is small, it can be observed and continued to take, if necessary, a small dose of estrogen can be added, if the amount is large, the drug should be discontinued, which is regarded as the current menstruation; Prolongation may be related to excessive local prostaglandin production or hyperfibrinolysis, and antifibrinolytic drugs are the first choice for treatment; women who have placed LNG-IUS or skin burial often occur within 6 months, and can be treated symptomatically or observed for a short period of time. At the same time to take short-acting contraceptives.
Uncategorized AUB
Individual patients with AUB may be related to other rare factors, such as arteriovenous malformation, uterine scar defect after cesarean section, myometrial hypertrophy, etc., but there is still a lack of perfect examination methods as a diagnostic basis, and these factors are classified as "unknown" Classification (AUB-N).
The causes of AUB caused by arteriovenous malformations are congenital or acquired (uterine trauma, post-cesarean section, etc.), most of which are sudden and massive uterine bleeding. The first choice for diagnosis is transvaginal ultrasonography. Other examination methods include uterine blood vessels. Angiography, pelvic CT and MRI examinations. In terms of treatment, oral contraceptives or expectant treatment can be used when the bleeding volume is not large. For patients with severe bleeding, to maintain stable vital signs, selective uterine artery embolization should be used as soon as possible. The pregnancy rate is low, and in addition to uterine vascular embolization, hysterectomy can be used for those without fertility requirements.
AUB caused by uterine scar defect after cesarean section is often manifested as prolonged menstrual period. The diagnosis method is transvaginal ultrasonography, and the best is hysteroscopy. Oral contraceptives can be used to shorten the bleeding time, and if the drug treatment is ineffective, surgical treatment may be considered, including hysteroscopic hysteroscopic diverticulectomy, laparotomy or laparoscopic scar tissue removal or repair around the uterine incision.
The above lists the common clinical symptoms of abnormal uterine bleeding in gynecology and the therapeutic effect of hysteroscopy in the above diseases. If the patient does not seek medical treatment in time at the early stage of the disease, the opportunity for minimally invasive treatment is lost, and the last option is to remove the uterus. Female friends must pay attention to gynecological examinations, and conduct regular gynecological examinations according to their own conditions, so as to detect diseases at an early stage and diagnose and treat them early. Once the clinical manifestations of the above-mentioned diseases appear, you should go to the regular hospital for treatment in time, so as to win the opportunity for the treatment of the disease, so as not to delay the disease and miss the best period of treatment.
Hysteroscopy is the application of dilatation media to dilate the uterine cavity, and the physiological and pathological changes of the cervical canal, internal cervical orifice, endometrium, and fallopian tube openings are observed through a speculum inserted into the uterine cavity, so as to directly and accurately sample the diseased tissue. Send pathological examination, but also can be directly treated under hysteroscopy.
- Recommended news
- 【General Surgery Laparoscopy】Cholecystectomy
- Surgery Steps of Hysteroscopy for Intrauterine Adhesion
- [Otolaryngology Otoscopic Section] Excision of Cholesteatoma in the External Auditory Canal
- [Otolaryngology Nasal Endoscopy] How to Treat Recurrent Rhinitis
- [ENT Surgery: Nasal Endoscopy] Endoscopic Treatment of Nasal Polyps